Insomnia and Neuroticism are Related with Depressive Symptoms of Medical Students
Article information
Abstract
Background and Objective
Insomnia is very common in depression and especially medical students are easy to experience sleep disturbance because of their studies. Also depressive symptoms are closely related to stress. Stress is an interaction between an individual and the environment, involving subjective perception and assessment of stressors, thus constituting a highly personalized process. Different personality traits can create different levels of stress. In this study, we tried to explore the relationship between insomnia and depressive symptoms or stress of medical students, and whether their personality may play a role on this relationship or not.
Methods
We enrolled 154 medical students from University of Ulsan College of Medicine. We used the Medical Stress Scale, the Multidimensional Perfectionism Scale, the Patient Health Questionnaire-9, the Academic Motivation Scale, the Insomnia Severity Index, and The revised NEO Personality Inventory (PI).
Results
Insomnia severity, amotivation, medical stress, mental health index and neuroticism traits of NEO-PI significantly correlated with depressive symptom severity (p < 0.001). And stepwise linear regression analysis indicated insomnia, amotivation and neuroticism traits of NEO-PI are expecting factors for students’ depressive symptoms is related to (p < 0.001).
Conclusions
Student who tend to be perfect feel more academic stress. The high level of depressive symptom is associated with insomnia, amotivation, academic stress in medical student. Moreover, personality trait also can influence their depressive symptoms.
INTRODUCTION
Researchers have studied the condition of depression as manifest in medical students for several decades. Depressive symptoms are closely related to perceived stress. Since there are various type of stressors present during any period of formal medical training [1], medical students are readily susceptible to depressive symptoms [2]. In recent study, 10% of medical students reported experiencing depressive symptoms, and majority of those individuals also reported suicidal ideation [3].
Medical students are also prone to sleep disturbance. Their sleep-wake cycle is frequently interrupted by delayed sleep onset and inadequate sleep duration, with secondary daytime somnolence and napping [4]. Their sleep deprivation might be related with lower academic performance [5]. Low academic performance causes stress, which causes anxiety and other symptoms, which causes insomnia and sleep deprivation, and the sleep deprivation further degrades the academic performance causing further stress and more insomnia. This becomes a vicious cycle [6]. However, the student’s innate and/or acquired ability to assess and adapt to significant academic stress depends on the personality type and/or coping strategies of the particular individual [7]. Stress is an interaction between the environment and the individual. Each person has his own personality, which includes subjective perception and coping strategies about stressors, so stress process is a highly personalized process [8].
Previous studies showed that personality traits are associated with mood symptoms. High neuroticism was reported to be associated with major depressive disorder, and low extraversion was correlated with dysthymia in general population [9]. Although psychological distress is a powerful predictor to depression among medical school students, their personality predispositions also affect depressive symptoms [10]. High level of neuroticism is a strong risk factor of major depression in Swedish twin study [11]. In Korea, medical students who have “avoidance” coping strategies tend to experience more stress than those who have other methods of coping with stress [12]. In addition, insomnia or sleep disturbance also may be influenced by individual’s personality. Harm avoidance and self-transcendence are positively related with insomnia. In contrast, novelty-seeking, reward dependence and cooperativeness are negatively related to severity of insomnia. Sleep quality is also correlated with self-transcendence [13].
Therefore, it is important to explore whether the insomnia symptoms of medical students influences their medical stress or depressive symptoms. In this study, we tried to explore the relationship between insomnia and depressive symptoms or stress of medical students, and whether their personality may play a role on this relationship or not.
METHODS
Participants
We enrolled 154 medical students ranging from the second year of pre-medicine through the third year of medical school at the University of Ulsan College of Medicine, and assessed their current academic stress and psychological problems such as sleep problem or depressive symptoms in 2015.
Before starting of the survey, we explained all details about the aims and methods of the study to the 159 students. We distributed printed questionnaires to the students, and requested that the students fill in them. Finally data of 154 students, who have consented, were included in the final analyses. The official approval of this study was authorized by the Institutional Review Board of the Asan Medical Center.
Measures
Students’ medical stress and academic motivation was assessed using the Medical Stress Scale (MSS) and Academic Motivation Scale (AMS). Their insomnia severity and depressive symptoms were checked using the Insomnia Severity Index (ISI) and Patient Health Questionnaire-9 (PHQ-9), Personality trait was assessed using the revised NEO Personality Inventory (NEO-PI) and the Multidimensional Perfectionism Scale (MPS).
The MSS is a self-report questionnaire to assess perceived stress levels in medical school [14], using a modified Korean version. The Korean version of the MSS consists of nine items focusing on three areas: school course of study and environment (four items); personal ability/perseverance (four items); and, and financial conditions (one item) [15]. Because all items had a 5-point answer, a total score is 45 points. Thus we set the cut-off point as 28 for the present research.
The AMS consists of a 28-item questionnaire to assess academic motivation [16] on the basis of self-determination theory [17] and it has three subcategories such as intrinsic motivation, extrinsic motivation and amotivation. Higher score represent higher levels of motivation in each subcategory. We used the validated Korean AMS version in the present study [15].
The ISI is a brief Self-Report Scale to evaluate the degree of both daytime and nighttime constituents of insomnia. The ISI consists of seven items to estimate the degree of sleep maintenance problems; sleep-onset difficulties and early morning awakening, satisfaction with his or her sleep state, influence on the functions of normal daytime life, severity of impairment of life of quality and level of concern caused by insomnia. All items have a 0–4 scale so the range of total score is from 0 to 28 (0–7: normal, 8–14: mild insomnia, 15–21: moderate insomnia, 22–28: severe insomnia) [18].
The PHQ-9 is an instrument about the assessment of depressive symptoms based on DSM-IV criteria. It was developed as a self-report version of the original PRIME-MD by Spitzer et al. [19] It consists of nine items about depressive symptoms, and there are one more question about functional impairment at the end of the diagnostic part of the PHQ-9: “How difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?” [20]
The revised NEO-PI evaluates personality based on the big five model. It has 240 questions and consists of openness to experience, conscientiousness, extraversion, agreeableness and neuroticism [21].
The MPS is a scale to assess the perfectionistic propensity. The MPS is invented by Frost et al. [22] in 1990. It has six subscales (excessive concern over making mistakes, high personal standards, perception of high parental expectations, perception of high parental criticism, doubting of the quality of one’s actions, and preference for order and organization) and 35 questions. Each item can be assessed using a 5-point Likert Scale, and total score can be calculated from 35 to 175. As the score is higher, we consider that the student’s perfectionism trait is stronger. In this study, the Korean version of MPS is used [23].
Statistical Analysis
A t-test of students has been used to make a comparison of the demographic and psychological characteristics between depressed students and non-depressed students. We also used Pearson’s correlation analysis to determine the relationship between depressive symptoms and carious other psychological variables. Based on these results, stepwise linear regression analysis has been performed to find the factor related to depressive symptoms. We used The Statistical Package for the Social Sciences version 21.0 (SPSS Inc., Chicago, IL, USA) for all statistical analyses.
RESULTS
Demographic and Psychological Characteristics of Participants
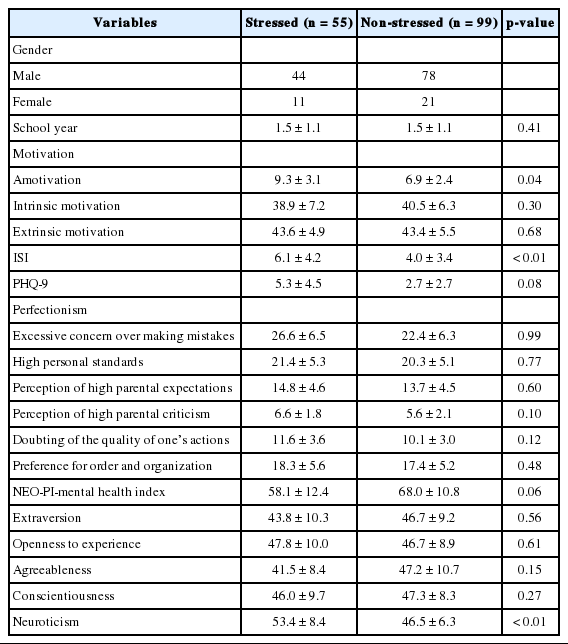
In our study group, only 32 (20.7%) students were female. Table 1 describes the demographic and psychological characteristics of the students grouped based on MSS score. In our participants, 29 (18.8%) students have insomnia (ISI score > 7). The ISI score is significantly high in stressed group (p < 0.01) compared to non-stressed group. Also we found that stressed group has higher score about neuroticism, one aspect of NEO-PI, than non-stressed group (p < 0.01). Statistically, there was no significant difference between the grades.
Correlation of Depressive Symptoms with Psychological Characteristics
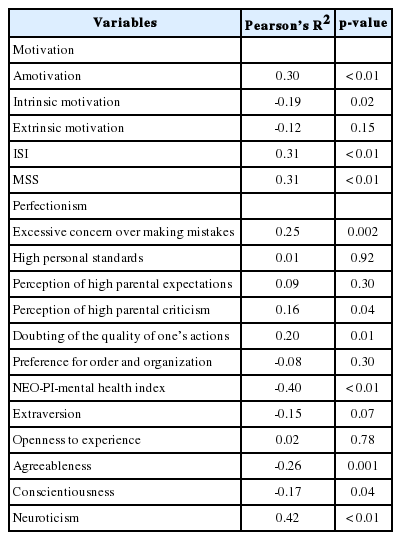
We performed Pearson’s correlation analysis to find out the association between depressive symptoms and other psychological characteristics (Table 2). ISI was found to be positively correlated with depressive symptom severity (p < 0.01). Also, we have found that MSS and amotivation were positively correlated with depressive symptom severity (p < 0.01). NEO-PI-mental health index and agreeableness trait were negatively correlated with PHQ-9 score (p < 0.01). Neuroticism trait was positively correlated with PHQ-9 score (p < 0.01).
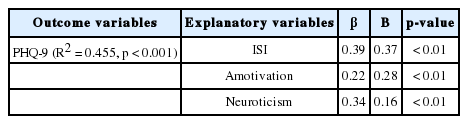
Next, based on these findings we have constructed stepwise linear regression model (Table 3). High ISI score, amotivation, and neuroticism trait were predictor variables for depression. Because of statistical result, all explanatory variables are highly reliable.
DISCUSSION
We proved that stress is significantly related with insomnia. We also determined that medical students who have neuroticism trait experienced more stress in medical school. Furthermore, we found that students who have high level of depressive symptoms tend to experience more insomnia and loss of motivation. Stress has a cause-and-effect relationship with depression, as shown by numerous previous studies. It became clear that chronic exposure to perceived stressors caused depression-like stress by making molecular, cellular, and behavioral changes [24]. Personality traits might also influence the severity of the depressive symptoms present. In stepwise linear regression model high ISI score, loss of motivation and neuroticism trait is a risk factor of symptom severity of depression of the students. Overall, insomnia and neuroticism trait of NEO-PI index are powerful factors related to experience depressive symptoms. In addition, motivation is importantly correlated with depression. According to our research, medical students who have sufficient and substantial motivation tend to experience less stress and fewer depressive symptoms.
Insomnia is closely linked to enrollment in medical school. There are already a proliferation of studies addressing the relationship between medical school, medical students and sleep disorders. In Asia, numerous researches were done to assess insomnia severity in medical students in China, Hong Kong, Malaysia, India, and Iran. In North and South America, United States, Brazil, and Mexico have epidemiological data on insomnia of medical students [25]. The attitudes, academic load, life style choices, potentially sleep apnea and internet usage may induce or exacerbate sleep disturbance [25]. Therefore, insomnia in medical students is considered a very important problem, worldwide.
Prior literary sources indicate document the belief that various psychiatric disorders have higher incidence and prevalence when the afflicted individuals suffer from insomnia. Insomnia patients are about four times more likely to develop depression than those who sleep well [26]. Besides, there are some research efforts showing that sleep problems would be a predictive factor of psychiatric disorder like alcohol abuse, anxiety or depression [26,27]. In addition, some researchers performed several studies about subgroups of insomniacs in past years. They prove that women, shift workers and those who simply don’t sleep enough are more vulnerable to insomnia [28]. As it has been concluded by previous researchers, our study reveals that insomnia is correlates significantly with depression. So if a medical student visits your office complains about sleep disturbance, it might be best if you look more closely and assess for other problems like symptoms of depression.
Our research indicates that some personality traits are related to depressive symptoms, too. Over previous decades, many researchers published papers documenting the possible relationship between personality and psychiatric disorders. In general population, the patient diagnosed with anxiety and depressive disorders will likely have more extraversion and neuroticism traits [10]. In meta-analysis including 175 studies, it was trait of “neuroticism” which was the most obviously and most often linked to the full spectrum of psychiatric disorders, and some other traits had considerable correlation apart from neuroticism [29]. In our study, the participants are all medical students, and some part of results was in line with the previous literatures.
Neuroticism is the propensity to experience pessimistic emotions, for example anxiety or sadness, including mood swings [30], and has been regarded as one of the personality traits which is related to psychopathology, especially depression and anxiety [31]. Researchers have focused on identifying potential the biological evidence linking neuroticism and mood symptoms. Some of them proved that neuroticism indicated quantitative trait loci on chromosomes 1, 4, 7, 12 and 13 [32] and another group of scientists revealed that serotonin transporter and gamma-aminobutyric acid(A) alpha 6 receptor variants are correlated with neuroticism [33]. However and to date, evidence of any biological basis to suggest, or indicate, a relationship between neuroticism and depression remains unclear (and controversial).
Motivation has been shown to affect the depressive symptoms in medical students. In medical school, there are various type of “stress” including “academic stress” [34]. When one considers the competitive climate which characterizes traditional medical school, it would be reasonable to assume that the medical students experience a substantial amount of academic stress. Thus, we might be well-served to consider establishment of a plan designed to decrease academic pressure to enhance motivation [35]. Furthermore, various types of approaches are needed to improve academic motivation, including social cognitive theory such as reinforce self-efficacy belief [36]. In present study, we also tested the partial link between the depressive symptoms and the trait of “perfectionism”, and a tendency toward self-doubt, the quality or correctness of one’s actions in retrospect. If necessary, a mal-adaptive “perfectionism” trait might be corrected for the sake of the mental health of the medical student in question.
There are several constraints in play in the current study. First of all, we had no means of verifying any of the participants’ self-described medical histories, especially when it came to the area of psychiatrics. If there was to be a large or disproportionate percentage of depressive disorder among our participants, it could adversely affect the raw data and the results. Second and as noted, this research is based on self-report questionnaires which contain subjective bias. However, the most of participants have experience to filling out questionnaires much like hours at some point during the last year. So they would be appropriately familiar with that process. Third, this was a cross-sectional study. So we could find the association between variables, but it was impossible to establish the causality. Forth, we didn’t accomplish the comparison about medical students and the students who have another major. In Korea, college students are in the most stressful situation including seeking a full-time job and student loan repayment. So the influence of insomnia and stress could be different to non-medical students. Furthermore there would be a personality difference between them. Further studies will be performed considering the possibilities.
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.