Comparison of Anti-Streptococcal Antibodies in Patients with Narcolepsy and Control Group
Article information
Abstract
Background and Objective
It has been reported that Streptococcal infection is probably a significant environmental trigger for narcolepsy patients from recent studies. However the relationship between the streptococcal infection and narcolepsy is not clear. The aim of this study is to explore the anti-streptolysin O (ASO) titer in narcolepsy patients and healthy control, and the associations of ASO titer levels and polysomnographic findings.
Methods
Sixty two narcolepsy patients and Fifty six healthy controls were recruited at the Sleep Center of St. Vincent’s Hospital. The multiple sleep latency test data and polysomnographic findings from the time of their diagnosis were reviewed. Disease duration was defined as the time between the first symptom and time of blood draw. HLA typing was also performed. Participants were tested for markers of immune response to β hemolytic streptococcus.
Results
Results indicated that titers of anti-streptococcal antibodies were not significantly different between patients with narcolepsy and healthy controls. There was no significant difference of ASO titer between the HLA DQB1*0602 positive group and HLA DQB1*0602 negative group. In narcolepsy with cataplexy patients, rapid eye movement sleep latency was significantly shorter in the ASO > 200 group.
Conclusions
There is no significant difference of ASO titers between patients with narcolepsy and healthy controls. The association between streptococcal infections and narcolepsy in Asian people may be not as significant as Caucasian people.
INTRODUCTION
Narcolepsy is a disabling disease typically characterized by excessive daytime sleepiness, mean sleep onset of less than eight minutes, cataplexy, sleep onset rapid eye movement sleep (REM) periods, and low cerebrospinal fluid hypocretin-1 levels. The prevalence is 2–10 per 10000 individuals in North America with higher prevalence reported in Japan. Men and women are equally affected and the symptoms usually present between the ages of 12 and 30 years, although onset at much younger and older ages have been reported. The disorder is unique because of its extremely close association with HLA-DQB1*0602 and hypocretin cell loss, suggesting autoimmune destruction.
Until recently, most narcolepsy studies have focused on narcolepsy with cataplexy, an etiologically homogenous disorder closely associated with hypocretin deficiency and HLA-DQB1*0602 positivity.1,2 Of narcoleptics with clear cataplexy, 85–93% are positive for HLA DQB1*0602, compared with 35–56% of narcoleptics without cataplexy.3,4
Environmental triggers have been explored as a stimulator of the autoimmune process of narcolepsy. A well-designed population-based study of narcolepsy has been initiated and found increased smoking exposure in patients with narcolepsy as a risk factor; the authors suggested the effect to be secondary to increased upper respiratory tract infections in secondary smoking.5 More recently, there was a report regarding Streptococcal infection as a significant environmental trigger for narcolepsy with cataplexy.6 In markers of the immune response to β hemolytic streptococcus such as anti-streptolysin (ASO) and anti-DNase-B (ADB) were the most highly associated to narcolepsy onset compared with controls and decreased with disease duration. In this study, we investigated ASO titer between narcolepsy patients and control group, and the associations of ASO titer level and polysomnographic findings.
METHODS
Subjects
Subjects with narcolepsy were recruited from outpatients and inpatients at the Sleep center of St. Vincent Hospital, South Korea between January 2010 and December 2011. Information collected for these subjects included demographics and clinical, biological, and polysomnography data.
International classification of Sleep Disorders, 2nd edition, was used as the basis for the diagnosis of narcolepsy with cataplexy and without cataplexy. Mild sleep apnea was not considered a criterion for exclusion providing it was not a primary cause of the daytime sleepiness reported. One subject of narcolepsy comorbid with mild obstructive sleep apnea was included, and there has been no clear evidence that mild obstructive sleep apnea affects the level of anti-streptococcal antibody titers. Patients with a diagnosis of secondary narcolepsy, multiple sclerosis, any autoimmune disease, head trauma, or any other neurological disorder were excluded.
Using this method, sixty two patients of narcolepsy were identified. Fifty six controls were selected from a pool of subjects to match each patient for race and geographic region. All cases of narcolepsy patients and controls did not show any clinical evidence of upper respiratory infections or sinusitis within the last 6 months at the time of blood draw. Disease duration was defined as time between the first symptom and time of blood draw for HLA typing.
All subjects gave written informed consent for the study, which was approved by the Institutional Review Boards. The presence or absence of DQB1*0602 was determined using DQB1 exon-2 sequence-specific primers.7
Assays
As β hemolytic streptococcus and Helicobacter pylori are known triggers of autoimmunity,8,9 we measured ASO titers as serologic markers of post-streptococcal status. These markers were assessed using commercially available kits (Roche, Germany) according to the manufacturer’s instructions.
Statistics
For an assessment of the normality of data, the Shapiro-Wilk test was performed before further analysis. Group comparisons of demographic, polysomnographic and multiple sleep latency test (MSLT) data were primarily made using Mann-Whitney U test. Analysis of covariance (ANCOVA) was performed to adjust confounding factors such as age difference. Comparisons of categorical variables were performed with Chi-square test or Fisher’s exact test. The Statistical Package for the Social Sciences (SPSS) 12.0 (SPSS Inc., Chicago, IL, USA) was used for these analyses. Statistical differences were considered significant at p value < 0.05.
RESULTS
Baseline Demographic and MSLT Data
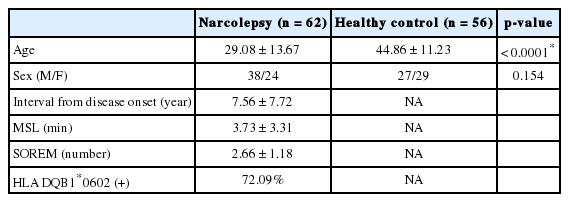
Table 1 show the baseline demographic and MSLT data in our different subject groups. There was no significant difference in sex between narcolepsy patients and the control group. However, the age of healthy controls is older than that of patients with narcolepsy (p < 0.0001). Mean sleep latency was 3.73 ± 3.31 minutes, number of sleep onset rapid eye movement (SO-REM) was 2.66 ± 1.18, interval from disease onset was 7.56 ± 7.72 years in narcolepsy patients. Percentage of positive HLA DQB1*0602 was 72.09% in groups of narcolepsy.
Anti-Streptolysin O
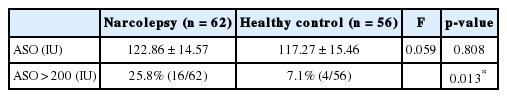
Titers of anti-streptococcal antibodies showed no statistically significant differences between patients with narcolepsy and healthy controls after adjusting the age as a covariate by AN- COVA. (122.86 ± 14.57 IU vs. 117.27 ± 15.46 IU, F = 0.059, p = 0.808, Table 2), The percentage of subjects whose ASO titer over 200 IU was significantly higher in patients with narcolepsy than healthy control (25.8% vs. 7.1%, p = 0.013, Table 2).
We analyzed the ASO titers in patients of narcolepsy with cataplexy (n = 42) and patients of narcolepsy without cataplexy (n = 20). There were no significant differences of ASO titer between patients of narcolepsy with cataplexy and patients of narcolepsy without cataplexy after adjusting the age as a covariate by ANCOVA (162.48 ± 30.17 IU vs. 150.93 ± 20.74 IU, F = 0.099, p = 0.755). The age between two groups was not significantly different (30.48 ± 14.01 vs. 26.15 ± 12.75, p = 0.247).
HLA DQB1*0602 and Anti-Streptolysin O
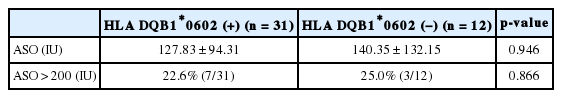
Of narcolepsy patients, 31 patients were HLA DQB1*0602 positive and 12 patients were HLA DQB1*0602 negative. There were no significant differences of ASO titer between the HLA DQB1*0602 positive group and HLA DQB1*0602 negative group (127.83 ± 94.31 vs. 140.35 ± 132.15, p = 0.946, Table 3) The percentage of subjects whose ASO titer over 200 IU was not significantly different between two groups (22.6% vs. 25.0%, p = 0.866, Table 3).
Anti-Streptolysin O and Polysomnographic Parameters
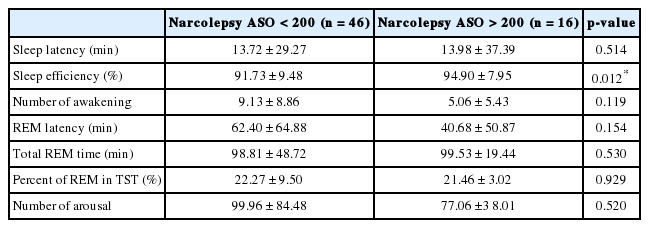
We subdivided narcolepsy patients into two groups, 46 narcolepsy patients with ASO titer below 200 IU and 16 narcolepsy patients with ASO titer over 200 IU. There were no significant differences between the two groups in sleep parameters; sleep latency, number of awakening, REM latency, total REM time, percent of REM in total sleep time, number of arousal, except sleep efficiency (91.73 ± 9.48% vs. 94.90 ± 7.95% p = 0.012)(Table 4).
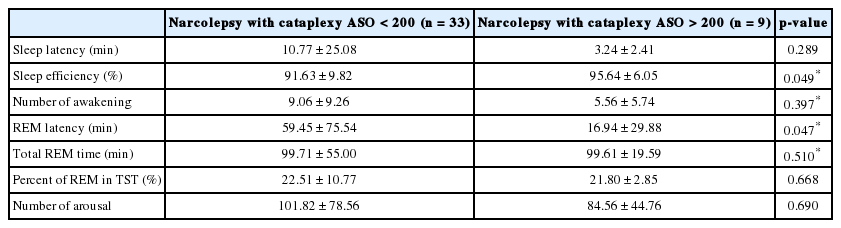
Of 62 narcolepsy patients, 42 patients were diagnosed as narcolepsy with cataplexy. We subdivided narcolepsy with cataplexy patients into 2 groups, 33 narcolepsy with cataplexy patients with ASO titer below 200 IU and 9 narcolepsy with cataplexy patients with ASO titer over 200 IU. Sleep efficiency was significantly higher in ASO > 200 group of narcolepsy with cataplexy (91.63 ± 9.82% vs. 95.64 ± 6.05%, p = 0.049, Table 5). REM latency was significantly shorter in ASO > 200 group of narcolepsy with cataplexy (59.45 ± 75.54 min vs. 16.94 ± 29.88, p = 0.047)(Table 5). There were no significant differences between the two groups in other sleep parameters; sleep latency, number of awakening, total REM time, percent of REM in total sleep time, and number of arousal.
DISCUSSION
Upper airway infections such as influenza and streptococcal infection may be common precipitants of a whole host of neuropsychiatric autoimmune complications including narcolepsy.
Recently, several studies suggested streptococcal infection or H1N1 infection could be triggering factors for the development of narcolepsy.10
Considering the association between genetic and environmental factors, it was presumed that ASO titer would be higher in narcoleptics than controls. A previous study by Aran6, reported that ASO and ADB titers were most highly close to narcolepsy onset (only subjects with cataplexy) and decreased with disease duration. But in our study, we found there is no significant difference of ASO titers between narcolepsy and controls. Our findings have several differences from the previous study:
The first one is that there is no significant elevation of ASO in both the cataplexy group and non-cataplexy group. Billiard et al.11 reported raised levels of anti streptococcal antibodies in narcolepsy subjects and Montplaisir et al.12 reported elevated levels of anti streptococcal antibodies in narcolepsy and idiopathic hypersomnia subjects. But our data is inconsistent with these studies. Rather, our results are consistent with a previous study by Matsuki et al.13 In this study, there were no significant differences of ASO titer between narcolepsy with cataplexy, hypersomnia, and normal controls. Futher, there might be different immunological responses to environmental triggers in Asian people. All reports of elevated ASO level in narcolepsy was performed for Caucasians, and the data for Asian by Matsuki et al.13 showed no significant elevation of ASO level. Other HLA subtype besides HLA DQB1*0602 could contribute to the onset of narcolepsy. DQA1*0102 and DQB1*0301 are known to increase susceptibility to narcolepsy whereas DQB1*0601 and DQB1* 0501 are protective.14,15 The role of these alleles to the exposure of streptococcal infection might be different in Asian people compared to Caucasians.
The second one is that high ASO titers are not associated with disease duration compare to the previous study which is correlated with close onset. In uncomplicated infections, anti-streptococcal antibodies are reported to increase after 2 weeks to peak 2–4 months and decrease thereafter.16 However, the long lasting antibody response in narcolepsy may thus reflect the special genetic background of these subjects and a sustained narcolepsy related immune reaction.17 Another consideration is diagnostic instability when we evaluate the effect of environmental factors on the onset of narcolepsy. Frequently, patients and family members don’t recognize the onset time of developing narcolepsy.
We found that HLA-DQB1*0602 is not associated with ASO titers. Similar results were reported by Eckhardt18 that no correlation was found between streptococcal antibodies and the presence of HLA-DR2 in the narcolepsy patient groups. It could be explained that streptococcal infections could simply make it permissive for other more specific factors rather than HLA to trigger narcolepsy, for example, by increasing blood brain permeability or simply reactivating the immune system nonspecifically.6
We also suggest higher ASO seems to influence the sleep quality measured by polysomnography; we found short REM latency in narcolepsy with cataplexy with high ASO (ASO > 200) group. Our study is the first report to evaluate ASO of narcolepsy including narcolepsy without cataplexy.
The limitations of this study are its retrospective design, and a small sample size. Also our study subjects have a difference of age among subgroups. The age of the patient is a very important factor in determining streptococcal antibody concentrations in a given population. Children between the ages of 6 and 15 years have the highest group A streptococcal antibody titers compared to very young children and older adults.19 But, we tried to adjust the effect of age differences by using ANCOVA, with age as a covariate.
Thus, the association between streptococcal infections and narcolepsy in Asian people may be not as significant as in Caucasian people and further studies are needed to explore the differences of immunological mechanisms.
Acknowledgments
We thank for all the patients who attended this study. Thanks to Dr. Mignot for his support in HLA typing and helpful comments.
Notes
Conflicts of Interest
The author has no financial conflicts of interest.