The Discrepancy-Cognitive Arousal Model of Insomnia Among the General Population
Article information
Abstract
Background and Objective
We aimed to explore the Discrepancy-Cognitive Arousal model among the general population, applying the discrepancy between desired time in bed and desired total sleep time (DBST index), dysfunctional beliefs about sleep, and sleep-related metacognitive processes.
Methods
An anonymous online survey study was conducted among the general population between January 10 and 18, 2022. The survey form included a questionnaire for demographic characteristics and rating scales such as Insomnia Severity Index (ISI), Dysfunctional Beliefs and Attitudes about Sleep–16 items (DBAS-16), and Metacognition Questionnaire for Insomnia–14 items (MCQI-14). In addition, questions for measuring participants’ DBST index were included.
Results
A total of 374 participants’ responses were analyzed. The ISI score was predicted by the DBST index (β = 0.11, p = 0.008), DBAS-16 (β = 0.37, p < 0.001), and MCQI-14 (β = 0.30, p < 0.001) in the linear regression analysis. In the mediation model, the DBST index directly predicted insomnia severity, and dysfunctional beliefs about sleep and sleep-related metacognitive processes mediated this relationship.
Conclusion
We observed that the Discrepancy-Cognitive Arousal model of insomnia was feasible among the general population.
INTRODUCTION
Insomnia is one of the most common psychiatric symptoms. Based on the cognitive model of insomnia, patients may have attention bias [1] for sleep-related cues, which may be extended to sleep-related worry. The worry for insomnia during the presleep period can induce attention bias for sleep-related negative information [2]. In addition, attention bias leads to misperception of sleep-wake cycle. Insomnia patients tend to go to bed early at night, since they believe that early bedtime facilitates easy sleep. However, based on two process models of insomnia, early bedtime does not guarantee an early sleep onset [3].
The DBST index, the discrepancy between desired time in bed (dTIB) and desired total sleep time (dTST), was proposed based on the insomnia patients who may desperately desire to sleep for a short period (dTST) despite unconsciously wanting to sleep for a substantial amount of time (dTIB) [4]. If a person desperately desires to sleep for at least 5 hours but desires to sleep from 10 pm until 7 am (9 hours of dTIB), we can speculate that he/she may have attention bias based on the 4 hours of discrepancy. Notably, we already observed that the high DBST index was correlated with severe insomnia among the general population [4] and cancer patients [5]. Based on the results of the previous studies, we can also speculate that a person who does not have sleep disturbance may have no discrepancy between dTIB and dTST (i.e., “I want to have 7 hours of sleep. For that, I usually go to bed 11 pm and wake-up 6 am.”). This suggests that the DBST index can predict attention bias, in insomnia patients.
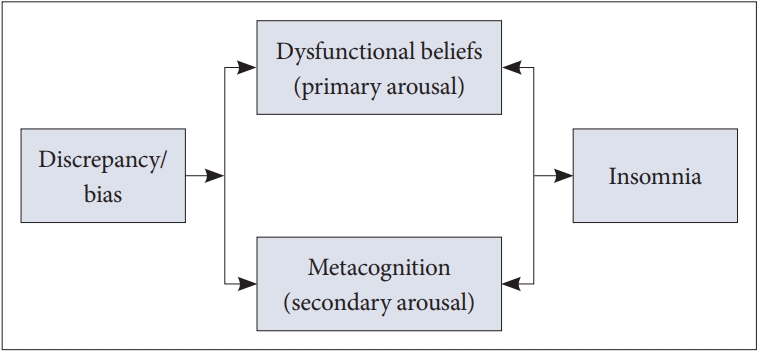
Ong et al. [6] proposed a metacognitive model of insomnia, which suggested a two-level model of arousal. Primary arousal includes thoughts or beliefs that interfere with sleep or daytime consequences of insomnia, which can be considered as dysfunctional beliefs about sleep [7], whilst secondary arousal includes emotional valence one assigns to sleep, which can be considered as the metacognitive process. Dysfunctional beliefs about sleep, as primary arousal, were reported to be associated with insomnia or poor sleep quality [8], as those beliefs contribute to aggravation of one’s arousal and influence the vicious cycle of dysfunctional beliefs-arousal-insomnia. As a secondary arousal, metacognition is characterized by the cognitive processes that occur in response to thoughts and cognition [6]. For example, worry about dysfunctional beliefs can amplify insomnia symptoms.
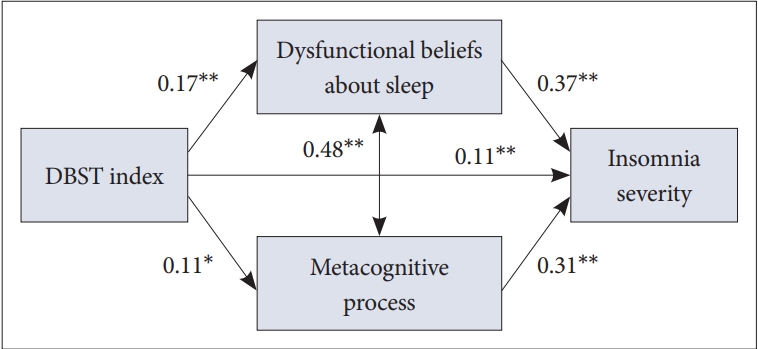
In this paper, we proposed a Discrepancy-Cognitive Arousal (DCA) model of insomnia (Fig. 1) and examined its feasibility among the general population. We considered that the DBST index could predict an attention bias in the cognitive model of insomnia. Furthermore, we hypothesized that the DBST index can predict insomnia in the two-level arousal model of insomnia with the mediation of dysfunctional beliefs about sleep and metacognition on insomnia.
METHODS
This analysis is part of a previous study [9] (Institutional Review Board of the Asan Medical Center, 2021-1755), which was done via an anonymous online survey conducted between January 10 and 18, 2022. Participants’ information on demographic characteristics and responses to rating scales were collected. Obtaining written informed consent from participants was waived by the Institutional Review Board. All 400 responses were estimated on the allocation of 40 samples for 10 cells (sex × five age groups). Enrolment emails were sent to 3000 registered panelists, 949 of them accessed the emails, 468 of them completed the process, and the first 400 responses were delivered to researchers at the survey company.
Rating Scales
DBST index
The participants’ DBST was calculated as (desired hours in bed)–(desired hours of total sleep time) [4]. A dTIB was estimated from participants’ responses to “From what time to what time do you want to sleep?” and dTST was estimated from their responses to “For how many hours do you want to sleep in a day?”
Insomnia Severity Index
The Insomnia Severity Index (ISI) is a self-rating assessment scale for an individual’s insomnia severity [10]. It includes 7 items which are scored on a 5-point Likert scale and the total score can range from 0 to 28. A higher total score indicates a severe degree of insomnia. Cronbach’s alpha in our sample was 0.801.
Shortened versions of Metacognition Questionnaire for Insomnia
The Metacognition Questionnaire for Insomnia–14 items (MCQI-14) is a shortened version of the original MCQ-I which can measure one’s metacognition on insomnia [11]. We validated the Korean version of MCQ-I, and developed shortened versions MCQI-6 and MCQI-14 by using the random forest machine learning technique [12]. In this study, we applied the Korean version of the MCQI-14, and Cronbach’s alpha among this sample was 0.906.
Dysfunctional Beliefs and Attitudes about Sleep–16 items
The Dysfunctional Beliefs and Attitudes about Sleep–16 items (DBAS-16) is a brief version [8] of the original DBAS scale [13], a self-rating assessment scale that can measure one’s dysfunctional beliefs about sleep. All 16 items in the DBAS-16 can be rated from 0 to 10, and the averaged total score can be calculated by summing up the scores of all the items and dividing by 16. A higher averaged score reflects a higher degree of dysfunctional beliefs about sleep. The Cronbach’s alpha was 0.898 among this sample.
Statistical Analysis
Variables were presented as mean ± standard deviation. Statistical significance was defined as two-tailed p-value of < 0.05. Pearson’s correlation coefficients were estimated among age and rating scales scores. Linear regression analysis with enter methods was conducted to explore variables for insomnia severity. The feasibility of the DCA model of insomnia was examined using mediation analysis implementing the bootstrap method with 2000 resamples. The SPSS version 21.0 (IBM Corp., Armonk, NY, USA), Amos version 27 (IBM SPSS, Chicago, IL, USA), and JASP version 0.14.1.0 software (JASP Team, Amsterdam, the Netherlands) were used for statistical analysis.
RESULTS
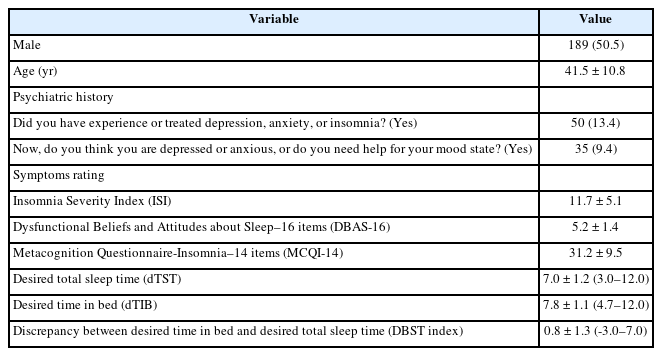
Among 400 responses collected from the participants, 26 participants who incompletely responded to the DBST index were excluded. Finally, 374 samples were analyzed. Table 1 shows the demographic characteristics and rating scales scores of this sample. Table 2 shows the correlation coefficients among the variables. There was no significant correlation between age and rating scales scores. The ISI was significantly correlated with DBAS-16 (r = 0.53, p < 0.001), MCQI-14 (r = 0.49, p < 0.001), and the DBST index (r = 0.20, p < 0.001). The DBAS-16 was significantly correlated with MCQI-14 (r = 0.50, p < 0.001) and DBST index (r = 0.16, p < 0.001). The MCQI-14 was significantly correlated with the DBST index (r = 0.11, p = 0.030).
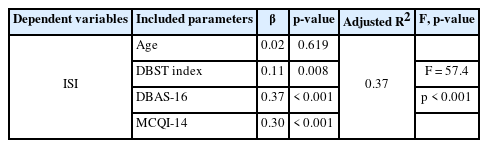
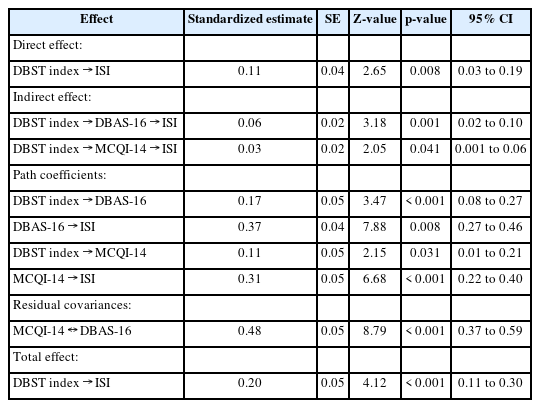
In Table 3, results from the linear regression analysis were used to predict variables for ISI scores. We observed that the ISI could be predicted by the DBST index (β = 0.11, p = 0.008), DBAS-16 (β = 0.37, p < 0.001), and MCQI-14 (β = 0.30, p < 0.001). Table 4 and Fig. 2 show the mediation analysis results. The DBST index was directly correlated to insomnia severity, and dysfunctional beliefs about sleep and sleep-related metacognitive processes mediated this relationship.
DISCUSSION
Our study results showed that the proposed DCA model of insomnia is feasible among the general population. The DBST index was directly correlated to insomnia severity, and dysfunctional beliefs about sleep and sleep-related metacognitive processes mediated the relationship.
In the cognitive model of insomnia, the importance of attention bias was reported [14]. Insomnia patients may misinterpret their sleep and daytime deficits; they underestimate sleep duration and overestimate daytime impairment [15]. In addition, an individual who has insomnia and is excessively preoccupied with sleep may have an attention bias to sleep-related information. The DBST index can be considered as one of the indicators of attention bias. In the previous reports, the DBST index was reported to be associated with insomnia severity [4,5]. Based on these results, theoretically, we can speculate that an individual who has a severe level of insomnia shows a high level of discrepancy between dTIB and dTST. Responses to the question on the DBST index of participants who have insomnia appear to have been given unconsciously. We observed that participants who did not have a high level of insomnia responded to the questions on dTIB as an estimate of the dTST; “In order to get 7 hours of sleep, I will go to bed at 11 pm and wake up at 6 am in the morning.” However, participants with insomnia answered questions unconsciously; unaware that there was a discrepancy between their responses to dTIB and dTST. Therefore, estimating the discrepancy between dTIB and dTST can be a simple and efficient way to measure an individual’s level of sleep disturbance and attention bias.
This is the first report to examine the association between the DBST index and sleep-related metacognitive processes. Metacognition, awareness or knowledge regarding one’s own mental state and cognitive processes, is the “thinking of thinking” process that influences the secondary cognitive arousal in a two-level model of arousal proposed by Ong et al. [6]. Secondary arousal concerns how insomnia patients react to their sleep-related beliefs, and it may magnify the negative emotional evaluation of sleep-related cognition in the primary arousal. Previous studies have shown that sleep-related metacognitive process is related to trait predisposition toward hyperarousal [16], and mediates the association between trait-hyperarousal and cognitive arousal [17]. Worry in the pre-sleep period, which is related to attention bias in insomnia patients [18], mediates the influence of the metacognitive process on sleep quality. A proper treatment using cognitive-behavioral therapy for insomnia CBT-I [7] can manage insomnia. Especially, it has shown that mindfulness and acceptance could be a tool for insomnia treatment [19]. The mediating effect of the sleep-related metacognitive process on the relationship between the DBST index and insomnia severity may increase the possibility of the DBST index as one of the predictors of attention bias.
In this study, dysfunctional beliefs about sleep also mediated the relationship between DBST index and insomnia severity. In a previous study, we observed that preoccupation with insomnia mediated the relationship between the DBST index and insomnia severity among the general population [4]. Preoccupation with sleep, measured with the Glasgow Sleep Effort Scale, and dysfunctional beliefs about sleep can be considered as the primary arousal component. The DBST index is not the same as dysfunctional beliefs about sleep, as the latter is a concept including faulty beliefs, worry, and attention bias, while the DBST index itself does not have concepts of dysfunctional beliefs or worry. We think that the discrepancy between dTIB and dTST only includes the unconscious bias of attention or interpretation. The results of this study show the possibility that the DBST index can be mediated by both of primary and secondary arousal components while predicting insomnia severity.
This study had limitations that need to be considered. First, evidence based on objective tests for the role of the DBST index in predicting attention bias was not provided in this study yet. Second, the survey was conducted via an anonymous online survey, and it is possible that the participants misunderstood the exact meaning of questions on the DBST index. Third, the small sample size is not enough to confirm that the DCA model is concrete. Therefore, further multicenter studies with large sample sizes are needed among various groups.
In conclusion, we observed the proposed DCA model is feasible among the general population, and that the possibility of the DBST index is an indicator of attention bias. We hope that this model can help to understand the characteristics of sleep-related cognitive processes in patients who suffer from sleep disturbance.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Author Contributions
Conceptualization: Seockhoon Chung. Data curation: Inn-Kyu Cho, Dongiin Lee, Jiyoung Kim, Eulah Cho. Formal analysis: Seockhoon Chung, Kayoung Song. Methodology: Seockhoon Chung. Project administration: Euah Cho. Supervision: Seockhoon Chung. Writing—original draft: Seockhoon Chung, Kayoung Song. Writing—review & editing: all authors.
Conflicts of Interest
Seockhoon Chung, the editorial committee chair of the Sleep Medicine Research, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Funding Statement
None
Acknowledgements
I would like to express my appreciation to all my team members and alumni of the Asan Medical Center sleep and psycho-oncology laboratory who guided me in developing the concept of the DBST index.