No Association Between Insomnia Severity, and Discrepancy Between Desired Time in Bed and Desired Total Sleep Time Among Shift-Working Nursing Professionals
Article information
Abstract
Background and Objective
This study aimed to explore whether the discrepancy between a patient’s desired time in bed and desired total sleep time (DBST index) can be used as a tool to assess the insomnia severity of shift-working nursing professionals.
Methods
Two studies were conducted during two different times among two groups of shiftworking nursing professionals working in COVID-19 inpatient wards (study I), or nurses who witnessed patient death during the previous 2 years (study II), using a single voluntary survey. The survey was completed by a total of 366 participants: 226 in the first study, and 140 in the second. Participants’ age, sex, marital status, and past psychiatric history were collected. In addition to questions regarding the DBST index, the Glasgow Sleep Effort Scale (GSES), Dysfunctional Beliefs about Sleep-2 items (DBS-2), and the Insomnia Severity Index (ISI) were assessed.
Results
In both studies, the DBST index did not reflect insomnia severity, preoccupation with sleep, or dysfunctional beliefs about sleep in the linear regression analysis. In addition, ISI was expected by GSES (β = 0.67 in study I, β = 0.62 in study II, all p < 0.001) and DBS-2 (β = 0.16 in study II, p = 0.020), but not by the DBST index.
Conclusions
It was observed that the DBST index was not significantly associated with insomnia severity, preoccupation with sleep, or dysfunctional beliefs about sleep in two studies done among shift working-nursing professionals.
INTRODUCTION
Many physical and psychiatric diseases can be caused by desynchronization of the biological clock in shift work. Shift workers typically experience fatigue and sleeplessness caused by a disrupted sleep–wake cycle, which is referred to as shift work disorder (SWD) [1]. According to the International Classification of Sleep Disorders, ICSD-3, excessive drowsiness or insomnia that happens as a temporary occurrence in relation to work schedules are the key symptoms of shift work sleep disorder. The term “shift work” refers to a variety of schedules, including regular night shifts, rotating shifts, permanent night shifts, and early morning shifts.
The SWD, one of the types of circadian rhythm sleep–wake disorder, is believed to arise from circadian rhythm and environmental stimulus misalignment, which could have negative effects on an individual’s health status and quality of life [2]. All of these factors affect individuals on a daily basis and other areas of their work and social lives. Studies have shown that many biological, behavioral, and cognitive factors are involved in the appearance of sleep disturbance. It was reported that shift work poses a higher risk for attention deficiency [3] or accidents while working [4,5], with the higher risk potential of night (28%) and evening shifts (15%), compared to day shifts [6]. On the other hand, a 2014 study showed that similar sleep profiles were presented in night shift workers, rotating shift workers, and day workers, where sleep time was more related to insomnia than to shift group type [7]. Workers with insomnia in all three groups suffered from anxiety, depression, and fatigue, and reported using equal amounts of sleep-aid medication [7].
Most people, including shift workers, would follow several measures to ensure a good night’s sleep, such as going to bed early to induce an early sleep onset. Nevertheless, this is not the case, as maintaining prolonged wakefulness is important for scheduled falling asleep in a timely manner, according to the two-process model that argues that sleep is regulated by the interaction between two processes: a homeostatic one (Process S), with a circadian pacemaker (Process C) [8]. This means that even when the circadian rhythm is sufficient, a homeostatic drive to fall asleep is needed to promote good sleep. We previously used a sleep index, namely “discrepancy between desired time in bed and desired total sleep time (DBST) index” [9]. The DBST index depends on the idea that people who suffer from insomnia want to sleep more and fall asleep earlier. They tend to go to bed earlier in the evening but wake up late in the morning as they struggle to fall asleep [9,10].
A high DBST indicates that the individual desires to sleep more, despite declaring that they require a short amount of sleep [9]. Arbitrating the effect of persistent preoccupation with sleep has long been found to be a fundamental factor for insomnia. Sleep preoccupation controlled the overall attributions for poor sleep, and in particular, sleep effort and sleep pattern problem attributions. According to Harvey’s model, many factors interact to increase insomnia; these include excessively negativelytoned cognitive activity, selective attention and monitoring, distorted perceptions, dysfunctional beliefs, and safety behavior [11]. These types of preoccupations with sleep start at the point of waking, and continue during the day, with people suffering from insomnia selectively observing their sensations of physical deficit throughout their day. Moreover, patients with insomnia tend to solve their perceived deficit by using compensatory behavior, like taking a nap or drinking a lot of caffeine. Such methods of compensation confirm the presence of sleep deficit and thus create a vicious cycle of negative mentality, leading to actual decrease in the individual’s daily functioning [9].
The relation of the DBST index to insomnia severity among the general population has already been explored [9], and also among cancer patients [10], who frequently suffer from insomnia during their cancer diagnosis and treatment trajectory. In contrast, no previous study has explored the relationship between the DBST index and the severity of shift workers’ insomnia. The aim of this study is to assess the DBST index among shift-working nursing professionals and explore whether it is associated with insomnia severity.
METHODS
Participants and Procedure
We examined the relationship between the DBST index and insomnia severity using data from two groups of healthcare workers, part of which research was reported previously [12,13].
The protocol of this analysis using two previous dataset (study I and II) was approved the Institutional Review Board of the Asan Medical Center (2023-0684).
Study I
During the period April 7th–26th of 2022, frontline nursing professionals working in COVID-19 inpatient wards of three tertiary hospitals affiliated with the University of Ulsan (Asan Medical Center in Seoul, Ulsan University Hospital in Ulsan, and GangNeung Asan Hospital in Gangneung, South Korea) were surveyed online. A voluntary survey was conducted, and the participants’ age, sex, and marital status were collected, but no identifiable personal information was collected. Their participation was rewarded with a gift coupon worth 10 USD. We targeted the collection of responses from 60% (n = 203) of all eligible nursing professionals working in COVID-19 inpatient wards (239 at Asan Medical Center, 150 at Ulsan University Hospital, and 50 at GangNeung Asan Hospital). After excluding inappropriate or incomplete responses, a total of 226 shift-working nursing professionals (121 in Asan Medical Center, 85 in Ulsan University Hospital, and 20 in GangNeung Asan Hospital) were analyzed. Study protocol approval was granted by the three Institutional Review Boards, which waived written informed consent (Asan Medical Center 2022–0323, Ulsan University Hospital 2022-01-06-003, and GangNeung Asan Hospital 2022-03-003-001).
Study II
During the period June 2nd–10th, 2022, an anonymous online survey was conducted at Asan Medical Center among doctors or nurses who witnessed patient death during the previous two years. As a reward, participants received a 5 USD gift coupon for completing this survey. The Institutional Review Board of Asan Medical Center approved the study protocol (2022-0740), and consent was waived. A voluntary survey was conducted, and participants’ age, sex, and marital status were collected, but no identifiable personal information was collected. Finally, after excluding inappropriate or incomplete responses, responses from nursing professionals who did not do shift work, and responses from medical doctors, all 140 shift-working nursing professionals were analyzed.
Measures
Insomnia Severity Scale
The Insomnia Severity Index (ISI) is a self-report rating scale that evaluates the severity, nature, and impact of insomnia [14]. It is made up of 7 items in total, where a 5-point Likert scale is used to rate each item, and where a higher total score indicates a more severe degree of insomnia. The scores are interpreted as follows: absence of insomnia (0–7); sub-threshold insomnia (8– 14); moderate insomnia (15–21); and severe insomnia (22–28).
Glasgow Sleep Effort Scale (GSES)
The Glasgow Sleep Effort Scale (GSES) is a self-report rating scale used to determine a person’s persistent preoccupation with sleep [15]. This scale is made up of 7 items rated on a 3-point Likert-like scale about how much patients are preoccupied with sleep, with the scores ranging from 0 (not at all) to 2 (very much), thus allowing the total score to range 0–14. A higher total score reflects a greater preoccupation with sleep.
Dysfunctional Beliefs about Sleep-2 items scale
The Dysfunctional Beliefs about Sleep-2 items scale (DBS-2) is a brief self-report rating scale [16] obtained from the C-DBS scale, originally developed in Korean, which is created to measure cancer patients’ dysfunctional beliefs about sleep. The DBS-2 scale consists of 2 items based on the questions: “My immune system will have serious problems if I don’t go to sleep at a certain time,” and “If I don’t sleep well at night, my health seems to be deteriorating.” Each item has a score ranging 0–10, with 0 being “strongly disagree” and 10 being “strongly agree,” where a higher total score means a higher level of dysfunctional beliefs about sleep.
Calculating the DBST index
The DBST index was determined as the difference between the patient’s desired total sleep time (dTST), which is estimated based on the response to the question, “For what hours do you want to sleep a day, if you do not do shift-work?” and the desired time in bed (dTIB), which is also estimated based on the response to the question, “From what time to what time do you want to sleep, if you do not do shift-work?” Finally, the DBST index was calculated as the difference between the desired hours of time in bed, and the desired hours of total sleep time: [desired hours of time in bed]–[desired hours of total sleep time] [9].
Statistical Analysis
The purpose of this study was to investigate whether the DBST index can be used to predict the severity of insomnia. To determine this, we examined the association of the DBST index with the rating scales of the ISI, GESE, or DBS-2 using Pearson’s correlation coefficients in two studies. A linear regression analysis with Enter method was conducted to explore expecting variables for the DBST index. In each study, demographic characteristics and rating scales scores were summarized as the mean±standard deviation. The significance level of the analyses was defined as two-tailed at a value of p < 0.05. The IBM SPSS Statistics, Version 21.0 (IBM Corp., Armonk, NY, USA) was used to perform statistical analysis.
RESULTS
Study I
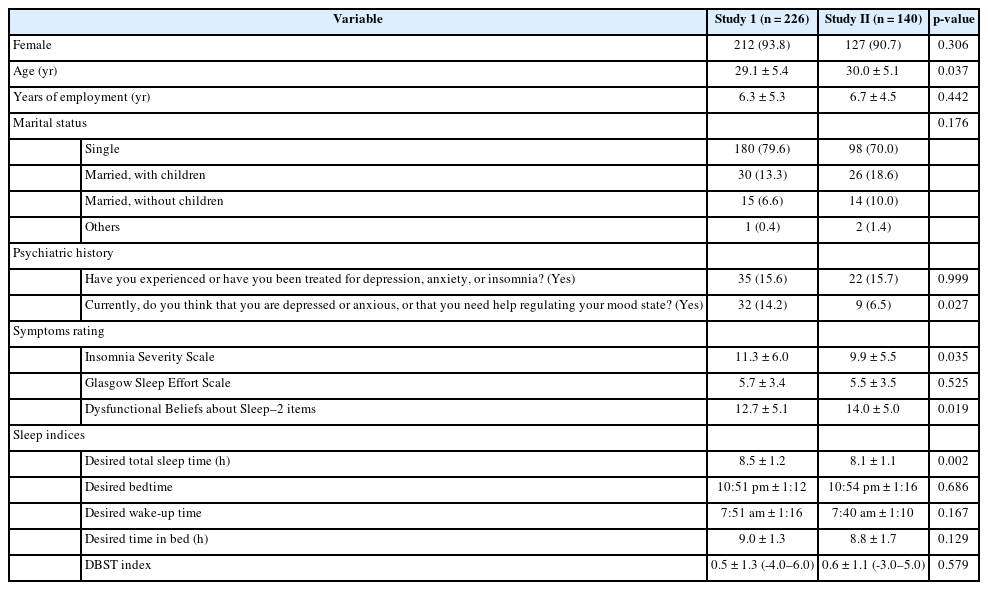
A total of 226 individuals were included in the first study (Table 1), the majority of whom were female (n = 212). A small percentage of 15.6% have had depression, anxiety, or insomnia, while 14.2% thought that they needed help regulating their mood state. Symptoms ratings included ISI with a mean of 11.3 ± 6.0, GSES with a mean of 5.7 ± 3.4, and DBS-2 with a mean of 12.7 ± 5.1. The sleep indices studied reported a dTST of 8.5 ± 1.2 h, desired bedtime of 10:51 pm ± 1:12, desired wake-up time of 7:51 am ± 1:16, dTIB of 9.0 ± 1.3 h, with DBST index of 0.5 ± 1.3 (-4.0–6.0).
Correlation coefficients of rating scale scores and the DBST index in study I (Table 2) showed there is no significant association of the DBST index with the ISI, GSES, and DBS-2 scores.
Linear regression analysis with Enter method among the shift working nursing professionals (Table 3) showed that the DBST index was not expected by age (β = 0.001, p = 0.984), ISI (β = 0.10, p = 0.306), GSES (β = -0.16, p = 0.105), and DBS-2 (β = 0.04, p = 0.587). Conversely, insomnia severity was expected by GSES (β = 0.67, p < 0.001) and DBS-2 (β = 0.10, p = 0.053).
Study II
A total of 140 individuals were included in the second study (Table 1), the majority also being female (n = 127). A small percentage of 15.7% had had depression, anxiety, or insomnia, and about 6.5% thought that they needed help regulating their mood state. Symptom ratings included ISI with a mean of 9.9 ± 5.5, GSES with a mean of 5.5 ± 3.5, and DBS-2 with a mean of 14.0 ± 5.0. Sleep indices studied reported a dTST of 8.1 ± 1.1 h, desired bedtime of 10:54 pm ± 1:16, desired wake-up time of 7:40 am ± 1:10, and dTIB of 8.8 ± 1.7 h, with DBST index of 0.6 ± 1.1 (-3.0–5.0).
Correlation coefficients of rating scale scores and the DBST index in study II (Table 2) showed that the DBST index was not significantly correlated with the ISI, GSES, and DBS-2 scores.
Linear regression analysis with Enter method among the shift working nursing professionals (Table 3) showed that the DBST index was not expected by age (β = 0.003, p = 0.977), ISI (β = 0.21, p = 0.084), GSES (β = -0.13, p = 0.278), and DBS-2 (β = 0.03, p = 0.751). Conversely, insomnia severity was expected by the GSES (β = 0.62, p < 0.001) and DBS-2 (β = 0.16, p = 0.020) (adjusted R2 = 0.48, F = 33.6, p < 0.001).
DISCUSSION
In this study, we investigated whether the DBST index was associated with insomnia severity in shift-working nursing professionals. The DBST index was not significantly associated with insomnia severity, preoccupation with sleep, or dysfunctional beliefs about sleep in the two studies. In a previous study of the general population [9], the DBST index was associated with insomnia severity and preoccupation with sleep, while preoccupation with sleep mediated the influence of dysfunctional beliefs about sleep and the DDBST index on insomnia severity. Among cancer patients [10], the DBST index was significantly associated with insomnia severity and sleep onset latency. However, we observed that contrary to expectation, the DBST index in two groups of healthcare workers was not significantly correlated with insomnia severity.
There is a possibility that a higher dTST in the current study may result in a non-significant result. The dTST in two studies (study I: 8.5 ± 1.2 h, study II: 8.1 ± 1.1 h) is relatively greater than that of the previous study (7.2 ± 1.2 h) [9]. In consequence, the DBST index was relatively lower (study I: 0.5 ± 1.3 [-4.0– 6.0], study II: 0.6 ± 1.1 [-3.0–5.0]) than that of a previous study (0.8 ± 1.4 [-2.5–7.0]). The DBST index concept is based on the idea that the discrepancy between dTIB and dTST may be greater if the individual is desperately in need of sleep, at least for a short period of time. This may lead to the non-significant correlation between the DBST index and insomnia severity.
It is also possible that the non-significance can be explained by the fact that the mean ages of these two studies (study I: 29.1 ± 5.4, study II: 30.0 ± 5.1) were younger than the mean ages of the previous studies [9,10]. In general, the total sleep time or sleep duration of older persons is reported to be shorter than that of younger persons [17]. Nursing professionals in younger age groups might need more sleep than middle-aged individuals in previous studies. A previous study conducted among the general population [9] found a significant correlation between age and dTST (rho = -0.25, p < 0.01). It is possible that the DBST index was ineffective in predicting insomnia severity among younger individuals, despite the fact that we cannot yet provide the data.
Another possible explanation is that participants were engaged in shift work, and responded that they needed to sleep more when they were not engaged in shift work. In this study, we asked nursing professionals for the dTST, “For what hours do you want to sleep a day, if you do not do shift work?” and for the dTIB, “From what time to what time do you want to sleep, if you do not do shift work?” Participants in this study were involved in shift work, which might have resulted in exhaustion, and they might have felt the need to sleep more when they were not engaged in shift work. As a result, when we asked the group what their dTST or TIB would be when they were not engaged in shift work, they might have responded with a relatively high dTST or TIB.
There are limitations to this study. First, the survey was conducted during the COVID-19 pandemic, and participants were likely to be caring for patients during a difficult time. Study I participants were working in COVID-19 inpatient wards, whereas study II participants had experienced patient death during the previous 2 years. It is possible for work-related stress or working environment to affect the response to dTSTs or TIBs. Second, this study was done via online survey, rather than through face-to-face interviews. Because the dTST and TIB were not regularly asked, there is a possibility that while responding to the online survey, participants misunderstood the meanings. Third, for the dTIB or TST, we asked participants, “If you don’t work shifts?” Participants had been working for approximately 6 years as shift workers in this study. Since they should posit that they were not shift workers, that might lead to bias.
In conclusion, the DBST index was not significantly associated with insomnia severity, preoccupation with sleep, or dysfunctional beliefs about sleep among shift-working nursing professionals in the two studies. Such results can be attributed to several reasons, including the young age group studied, a higher dTST in the two study populations, and finally the fact that the participants from both studies responded that they needed to sleep more when they were not engaged in shift work. Further studies are needed to confirm or counteract this finding, since insomnia and sleep disturbance can influence an individual’s quality of life, especially nurse shift workers, whose work is indispensable for the health of others.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Authors’ Contribution
Conceptualization: Seockhoon Chung. Data curation: Seockhoon Chung. Formal analysis: Kikyoung Yi, Seockhoon Chung. Methodology: Wafaa Bzeih, Sohyeong Kim. Project administration: Seockhoon Chung. Writing—original draft: all authors. Writing—review & editing: all authors.
Conflicts of Interest
Seockhoon Chung, the Editorial Committee Chair of Sleep Medicine Research, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Funding Statement
None