A Single Center Study of the Clinical Features and Comorbidities of Patients with Restless Legs Syndrome
Article information
Abstract
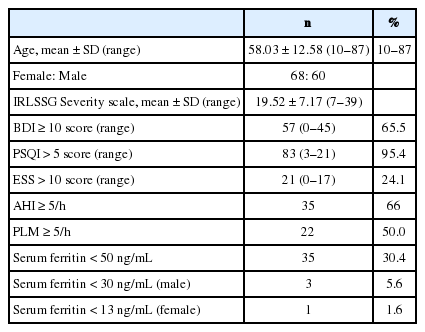
This study investigated the clinical features and comorbidities of patients with restless legs syndrome (RLS). A total of 128 RLS patients (68 women, 60 men; mean age = 58.03 ± 12.58 years) were assessed. The severity of RLS was evaluated by the International RLS Study Group (IRLSSG) Severity Scale. Among the subjects with RLS, depressive symptoms (65.5%) and poor sleep quality (95.4%) were frequently reported, and 88.3% of the patients showed moderate-to-severe symptom severity on the IRLSSG Severity Scale. The most common complaint was insomnia (70.3%), and 16 patients (12.5%) reported leg discomfort as their main symptom. Obstructive sleep apnea was observed in 66% of RLS patient. Iron deficiency was not prevalent in RLS patients. The severity of RLS was not significantly correlated with depression, sleep quality or sleepiness. We conclude that when assessing insomnia patients, RLS symptoms should be evaluated.
INTRODUCTION
Restless legs syndrome (RLS) is characterized by discomfort in the legs, which might be creeping, crawling, tingling, or painful in nature.1 These symptoms are worse at rest, are relieved by movement, and mainly occur in the evening or night. Because of this, RLS patients complain that they have difficulty in falling asleep or maintaining sleep.2,3 Additionally, these symptoms are connected to fatigue, depressive mood, damaged working ability, and social isolation.4,5 Epidemiological studies have demonstrated that the symptoms of RLS are present in about 5–10% of the general population.2,6 Nevertheless, proper treatment has not always been conducted for the symptoms of RLS because of low recognition or under diagnosis of the disease.7 To widen knowledge of the syndrome in Korea, more clinical experience and studies are necessary. There have been few studies in Korea in which idiopathic RLS patients have been studied for clinical features. This study was therefore conducted to determine the severity level of patients with RLS by using the RLS severity scale developed by the International RLS Study Group (IRLSSG), and to further examine the relationships between RLS severity and sleep quality, daytime sleepiness and depression. In addition, iron metabolism changes and nocturnal polysomnography (NPSG) characteristics were studied.
METHODS
We have performed a retrospective study of 128 patients with RLS who were seen in a sleep clinic. In the present study, we included patients who visited the sleep clinic of Seoul National University Bundang Hospital from March 2004 to July 2007, and who satisfied the four diagnostic criteria for RLS.8 We excluded patients with conditions causing secondary RLS such as chronic renal failure, diabetes mellitus, Parkinsonism or pregnancy. The study protocol was approved by our Institutional Review Board.
The criteria for RLS used in this study were as follows; 1) an urge to move the legs, usually accompanied or caused by uncomfortable and unpleasant sensations in the legs; 2) the urge to move or the beginning or worsening of unpleasant sensations during periods of rest or inactivity, such as lying or sitting; 3) symptoms can be partially or totally relieved by movement, such as walking or stretching, at least as long as the activity continues; 4) symptoms are worse in the evening or night than during the day or occur only in the evening or night.1 The severity of RLS was evaluated by IRLSSG Severity Scale.8 This rating scale consists of 10 questions, with each question having 5 scores (0–4 scores). RLS severity is obtained after amalgamating the scores for each question (0: no symptom; 1–10: mild; 11–20: moderate; 21–30: severe; 31–40: very severe). Perceived sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI).9 Depressive symptoms and daytime sleepiness were evaluated by the Beck Depression Inventory (BDI),10 and the Epworth Sleepiness Scale (ESS).11 To assess iron deficiency, iron and ferritin were measured from serum. NPSG was performed on 53 patients in the sleep laboratory of Seoul National University Bundang Hospital during one night. The Embla N 7000 recording system (Medcare®) and the analytic tool Somnologica (version 3.3.1) were used. Based on the criteria of Rechtschaffen and Kales,12 sleep was scored for every 30-second epoch of the NPSG. Statistical analysis was carried out using Statistical Package for the Social Sciences 12.0. Statistical significance was defined at the level of p < 0.05. Data were expressed as mean ± standard deviation. Analysis of variance was performed for statistical evaluation of the differences in BDI, PSQI and ESS according to the severity of RLS.
RESULTS
From the 128 RLS patients studied, the most common complaints on initial visit were insomnia (n = 90, 70.3%), abnormal leg sensation (n = 16, 12.5%). Other complaints were anxiety, dream enactments, panic attacks, depressive mood and loud snoring. Our subjects comprised 60 men (46.9%) and 68 women (53.1%) with average age of 58.0 ± 12.6 years. Most (88.3%) had symptom severity at or beyond a moderate degree. The specific RLS severity scores were as follows: 10 patients (7.8%) had very severe symptoms; 43 patients (33.6%) severe; 60 patients (46.6%) moderate; and 15 patients (11.7%) had a mild severity level. For BDI scores, the proportion of patients with scores above 10 (the cut-off for depression) was 65.6%, and 95.4% of patients had PSQI global score above 5 (the cut-off for poor sleep quality). The proportion of patients with daytime sleepiness was 24.1% (Table 1). NPSG results from 53 RLS patients are shown as Table 1. Of these, the number of patients with more than 5 on the apnea-hypopnea index was 35 (66%), and the number of patients who displayed more than 5 on the periodic limb movements during sleep (PLMS) index was 22 (50%). Of the 115 patients whose serum we examined, 35 (30.4%) had a serum ferritin level lower than 50 ug/dL. Three (5.6%) male had a level of lower than standard 30 ng/mL, whereas one (1.6%) woman had serum ferritin level below the standard 13 ng/mL (Table 1). Patients were categorized into four groups based on their severity level: mild, moderate, severe and very severe. BDI, PSQI and ESS scores were higher in the very severe group, but differences between groups were not statistically significant. There was no significant correlation between serum ferritin and IRLSSG (r = −0.081 p = 0.391) or between serum ferritin and PLMS (r = 0.045, p = 0.754).
DISCUSSION
Among the RLS patients in this study, only 16 (12.5%) reported leg discomfort as their chief complaint, with 70.3% of patients complaining of insomnia as their chief problem. This finding might be related to the low recognition of RLS and the high prevalence of sleep problems in RLS patients. RLS has become an increasingly well-known sleep disorder in recent years, but during the study period of March 2004 to July 2007, patients would have been unlikely to visit a sleep clinic complaining of leg discomforts because of low awareness RLS in Korea. In a 2004 study, it was found that 102 out of 103 patients did not realize that they had RLS due to a lack of information about the syndrome.13 Another study found that 79% of RLS patients complained of insomnia and had difficulty in falling asleep or maintaining sleep.14 The average IRLSSG severity score in this study was 19.52 ± 7.1, which is comparable to 2007 study which found a mean IRLSSG severity score of 23.6 ± 6.7 among 200 idiopathic RLS patients who had not received any treatment.15 Most of the RLS patients in the current study needed treatments given that 88.3% of them had an at least moderate severity level. Taken together, these results indicate that it is necessary to perform face-to-face interviews and to assess RLS symptoms for patients who complain of insomnia in clinical settings.
The proportion of patients who showed depressive symptoms in this study was 65.5%. RLS patients can sometimes mistakenly understand their RLS symptoms as those of depression.16 Although RLS patients are likely complain of fatigue, insomnia, and decreases in concentration, these symptoms could all be explained as symptoms of depression rather than RLS.17 The close relationship between RLS and insomnia in this study could explain the high prevalence of depressive symptoms in RLS. The degree of depression and anxiety is known to be higher for people with insomnia than for those without.18
In this study, sleep apnea syndrome (SAS) was observed in 35 of the 53 RLS patients (66%) examined with PSG. Lakshminarayanan et al.19 reported that the proportion of RLS patients was 2.5% in the control group, but it was 8.3% in patients with SAS. He suggested that all the patients who undergo NPSG should be evaluated for RLS symptoms. Considering the reported high prevalence of RLS in SAS patients, other factors should be noted regarding this relationship in our study. That is, we used relatively older population with an average age of 58 years and we performed NPSG only for patients who complained of snoring. These factors might explain the close relationship between RLS and SAS that our study found. On the other hand, PLMS was shown in 50 % of RLS patients in this study, which is relatively low, considering that a previous study reported an 80.2% comorbidity of PLMS with RLS.20 Given that we performed NPSG on only one night, a lower prevalence of PLMS might have been expected, because PLMS is not observed every day,21 and it is therefore necessary to measure PLMS repeatedly over several days.
The proportion of patients with serum ferritin levels below 50 ng/mL was 30.4%, and the proportion of patients with lower ferritin than the normal value was 5.6% in men, and 1.6% in women. Previously, it was reported that the worse the RLS symptoms, the lower the serum ferritin level,22 but a significant relation between RLS severity and ferritin level was not found in this study. Recently, it was proposed that there is no difference in the blood serum ferritin of RLS patients in comparison to a control group,23,24 Due to these conflicting result, it is necessary to research further into peripheral iron abnormality in primary RLS patients to assess whether iron should be provided to RLS patients with serum ferritin levels lower than 50 ng/mL.
This study has several limitations. As we had no control group without RLS, the characteristics of RLS patients could not be contrasted with a healthy population. In addition, as the study subjects were all patients who came to the sleep clinic of specific university hospital, caution needs to be taken in generalizing the study results. That is, the RLS patients in this study had higher severity levels and comorbidities compared to patients in the community. Lastly, we did not use standardized Korean versions of International RLS severity scale and ESS, which might lessen the validity of this study.
In conclusion, a large number of RLS patients visiting our study’s sleep clinic complained principally of insomnia, and most of them had moderate-to-severe degree of RLS severity. Therefore, when patients visit clinicians complaining of insomnia, clinicians are encouraged to assess for RLS by asking questions about leg discomforts.
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.