Challenges in Diagnosing Narcolepsy and Idiopathic Hypersomnia
Article information
Abstract
Narcolepsy and idiopathic hypersomnia are central disorders of hypersomnolence accompanied by excessive daytime sleepiness, which are not caused by nocturnal sleep disturbance, sleep deficiency, or circadian rhythm sleep disorders. Several studies have questioned the repeatability of the Multiple Sleep Latency Test (MSLT) in type 2 narcolepsy (NT2) patients. After two or more repeated MSLTs, the diagnosis of type 1 narcolepsy (NT1) is maintained in more than 90% of cases, while only half of the NT2 patients retain their original diagnosis. The diagnosis of NT2 may shift to idiopathic hypersomnia based on the MSLT results, making the differential diagnosis of NT2 and idiopathic hypersomnia particularly challenging. Therefore, this study suggests the need for new tests in addition to the MSLT for diagnostic consistency in NT2 and idiopathic hypersomnia.
INTRODUCTION
Narcolepsy and idiopathic hypersomnia are central disorders of hypersomnolence, characterized by excessive daytime sleepiness (EDS) in the absence of nocturnal sleep disturbance and sleep deficiency [1-4]. However, some narcolepsy cases are distinguished from idiopathic hypersomnia by the presence of cataplexy [5-12].
Cataplexy is associated with the pathophysiology of narcolepsy [1,6]. Narcolepsy occurs owing to the HLA-DQB1*0602 gene, which activates the immune system under certain environmental factors, such as infections, and destroys hypocretin-producing cells in the lateral ventricle of the brain [1,13-22]. Concordantly, the 3rd edition of the International Classification of Sleep Disorders includes hypocretin levels lower than 110 pg/mL and the presence of cataplexy in the diagnostic criteria for type 1 narcolepsy (NT1), whereas type 2 narcolepsy (NT2) can be diagnosed without cataplexy or low hypocretin levels [4].
Because measuring hypocretin levels is too invasive and of limited use, diagnosing narcolepsy mainly relies on the Multiple Sleep Latency Test (MSLT) [23-26]. The diagnostic criteria for NT1 and NT2 are the same for the MSLT, with a mean sleep latency of ≤ 8 minutes and ≥ 2 sleep-onset rapid eye movement (SOREM) episodes, while that of idiopathic hypersomnia varies by a sleep latency of ≤ 8 minutes but with ≤ 1 SOREM episodes [4,19,24,25,27-32].
Nevertheless, the validity of the MSLT has been questioned for NT2 and idiopathic hypersomnia [26,33-39]. This article reviews studies in which the diagnosis of NT2 and idiopathic hypersomnia has been changed by repeated MSLTs and discusses the potential causes and countermeasures for these diagnostic shifts.
REPEATABILITY OF MSLT IN NARCOLEPSY AND IDIOPATHIC HYPERSOMNIA PATIENTS
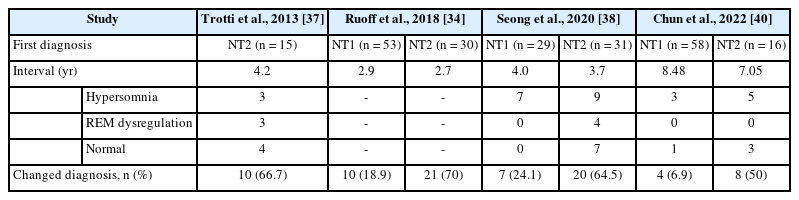
When the MSLT was retested in NT1 patients at intervals of 2.7–8.5 years, 73.9%–93.1% of the diagnoses were concordant with the original diagnosis, although in case of NT2 patients, only 30%–50% of the diagnosis remained consistent (Table 1) [34,37,38,40]. In the follow-up MSLT of NT2 and idiopathic hypersomnia, a considerable number of NT2 cases were converted to idiopathic hypersomnia (3/15 in Trotti’s study [37], 9/31 in Seong’s study [38], and 5/16 in Chun’s study [40]), while others were converted from idiopathic hypersomnia to NT2 (1/14 in Trotti’s study [37]). In 2013, Trotti et al. [37] showed that only 5/15 NT2 patients and 8/14 idiopathic hypersomnia patients maintained their diagnosis when the MSLT was repeated with an interval of 4.2 years.
This corroborates that the diagnostic value of MSLT in NT1 is reliable over time, whereas it is unreliable in NT2 [33-38,41]. This disparate repeatability of the MSLT results may be owing to the different progression patterns of NT1 and NT2 [37,38,40]. Specifically, symptoms or scorings may shift in NT2 and idiopathic hypersomnia patients, as their propensity for EDS and SOREM varies throughout the years, whereas NT1 remains consistent with hypocretin deficiency and cataplexy [36-38].
POSSIBLE EXPLANATIONS FOR THE POOR REPEATABILITY
There are a few possible reasons for these diagnostic shifts. MSLT results may have been influenced by undisclosed sleep problems. Sleep deprivation, obstructive sleep apnea, circadian rhythm disorder, or shift work can result in two or more SOREM episodes [36,37,39,42]. For the accuracy of the results and to rule out other sleep disorders, the patients were asked to complete a sleep log for 2 weeks, undergo actigraphy, and list their medications ahead of the MSLT.
Patients with previously diagnosed EDS, who subsequently showed improvement in their symptoms and tested normal on MSLT, may have been misdiagnosed with NT2 during their initial MSLT [34,37,38]. The presence of other aforementioned sleep disorders may have confounded the initial diagnosis.
Another reason would be that MSLT was performed incorrectly because of poor testing conditions or continuation of stimulant drugs. The amount and quality of sleep during the night before the MSLT, as well as the ability to stay awake between tests, need to be strictly controlled [34,37,40]. Thus, stimulant medication may delay sleep latency. The MSLT results were only accurate if the medication was discontinued for 2 weeks before the test. However, the patients may have continued to take the medication despite these instructions, as staying awake without medication may have been difficult during the day.
Finally, the MSLT results could have been misinterpreted. For example, in some cases, rapid eye movement is seen in only one 30 second-epoch and could have been missed while scoring [42].
CONSEQUENCE OF THE DIAGNOSTIC SHIFT
Diagnostic shifts caused by poor repeatability of MSLT could negatively impact patients’ understanding of their symptoms and curtail their ability to cope with their chronic disease by losing trust in healthcare providers.
Moreover, under current guidelines, if patients who were formerly diagnosed with and treated for NT2 show ≤ 1 SOREM at retest, they can no longer be diagnosed with narcolepsy. This causes diagnostic confusion but also a major difference in a patient’s therapeutic options. Unlike narcolepsy, the insurance company of the South Korean government does not cover the medical expenses for treating idiopathic hypersomnia. The patient would still need narcolepsy medications, including Provigil, Nuvigil, and Wakix, as they would continue to experience the same EDS symptoms.
STRATEGIES FOR MINIMIZING THE RISK OF MISDIAGNOSIS IN TYPE 2 NARCOLEPSY PATIENTS
To overcome the limitations of the current diagnostic standards and methods, we suggest: 1) repeating MSLT at intervals of ≥ 3 months, 2) meticulously ruling out other sleep disorders with EDS from narcolepsy at the first visit, and 3) identify the pathophysiology of NT2 and idiopathic hypersomnia [34,37,38,40].
CONCLUSION
As such, the MSLT has limitations in diagnosing NT2 and inconsistencies in follow-up tests. Precise diagnosis of NT2 requires careful attention to diagnostic complications and appropriate test conditions. It is highly recommended to repeat the MSLT and further develop more accurate diagnostic methods to reduce unwanted diagnostic shifts. The differential diagnosis of NT2 and idiopathic hypersomnia solely relying on MSLT should also be improved, as it could undermine the diagnostic classification of narcolepsy and hinder the accurate research of narcolepsy.
Notes
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
Authors’ Contribution
Conceptualization: Seung-Chul Hong. Investigation: Seung-Chul Hong, Tae-Won Kim. Methodology: Seung-Chul Hong. Project administration: Seung-Chul Hong, Tae-Won Kim. Visualization: Young-Chan Kim. Writing—original draft: Seung-Chul Hong, Young-Chan Kim, Ji Hyun Song. Writing—review & editing: Seung-Chul Hong, Ji Hyun Song.
Conflicts of Interest
Seung-Chul Hong, a contributing editor of the Sleep Medicine Research, was not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Funding Statement
None.