Differences in Trauma-Related Guilt in Females with History of Sexual Violence Based on Insomnia Severity
Article information
Abstract
Background and Objective
Females with history of sexual violence report a high percentage of insomnia. Guilt is a common symptom among this group. This study investigated differences in trauma-related guilt cognition between females of sexual violence with high or low symptoms of insomnia.
Methods
Participants were 43 females who reported having a history of sexual violence (mean age 26.56±7.81). All participants completed questionnaires about insomnia symptoms (Insomnia Severity Index, ISI), Posttraumatic stress disorder (PTSD) symptoms (PTSD Symptom Scale Self-Report), trauma-related guilt (Trauma-related Guilt Inventory, TRGI), depression (Beck Depression Inventory) and trauma-related information. The TRGI is consisted by global guilt, distress and guilt cognitions. Guilt cognitions can further be divided into Hindsight-Bias/Responsibility, Wrongdoing, and Lack of Justification subscales. Analyses were conducted using Pearson’s correlation coefficient and analysis of covariance.
Results
Results indicated ISI scores were significantly positively associated with PSS scores (r = 0.620, p < 0.01) and the distress subscale of the TGRI (r = 0.488, p < 0.01), and negatively associated with guilt cognitions (r = −0.423, p < 0.01). 53.5% (n = 23) of the sample met criteria for clinical insomnia using ISI cut-off scores of 15. Participants in the insomnia group scored significantly lower in overall guilt cognitions (p < 0.001) and significantly higher in distress (p = 0.001) than the non-insomnia group after controlling for depression. Among the subscales of guilt cognitions, hindsight-bias/responsibility was significantly lower in the insomnia group (p < 0.001).
Conclusions
Guilt can sometimes be adaptive in trauma patients as it may work as a catalyst in cognitively processing their trauma. Our results indicate that individuals with insomnia report lower guilt cognition. This may subsequently interfere with their ability to process the traumatic experience and effectively cope with their situation.
INTRODUCTION
Posttraumatic stress disorder (PTSD) is a psychological disorder that can occur after a traumatic experience or witnessing a shocking event. According to the National Co-morbidity Survey, the lifetime prevalence of PTSD was approximately 6.8% [1]. Patients with PTSD often experience several physical and psychological symptoms, with sleep disturbance being one of the most prominent symptoms. Sleep-related symptoms of patients with PTSD include sleep onset and maintenance difficulties and frequent nightmares as a result of traumatic events [2]. Subsequently, sleep difficulties such as insomnia can affect the onset and maintenance of PTSD symptoms [3]. Additionally, exposure to certain types of trauma such as sexual trauma, physical assault, and sudden death is associated with two-to three-fold increased risk of insomnia [4]. According to Steine et al. [5], individuals who were sexually abused reported more frequent sleep problems compared to non-abused individuals. Among them, the incidence of sleep disorder symptoms was especially high in rape and sexually abused victims.
The majority of theories suggest that cognitive and emotional responses play an important role in the development and maintenance of PTSD after trauma. Guilt may be especially relevant in the process of dealing with post-traumatic events [6]. Trauma-related guilt is an emotion that involves an evaluation of one’s role in a negative event. In particular, guilt involves a negative assessment of a particular behavior, such as “I should have known better.” A negative perception of their role after the trauma event may temporarily contribute to PTSD symptoms. However, it is less painful over time because the assessment of their role affects the process of dealing with the trauma [7]. Trauma related Guilt could be related to subsequent trauma-related sleep disturbance [8].
According to Ham et al. [9], chronic insomnia patients tend to have higher guilt-proneness. This characteristic suggests that guilt is particularly salient among those experiencing chronic insomnia. Prior research has not, however, specifically investigated the role of trauma-related guilt in PTSD patients with insomnia. In theory, traumatic events cause conflicts in the process of integrating individuals with their schema and their misbehavior. These conflicts are related to sleep disturbances [8]. Thus, the current study aimed to investigate the differences in trauma-related guilt cognitions between females of sexual violence who reported high and low symptoms of insomnia.
METHODS
Participants and Procedures
Participants were 43 females who were victims of sexual assault, ranging in age from 18 to 49 years old. All participants were recruited into the study after visiting the Sunflower Center of Southern Gyeonggi province, a trauma center specifically for females of sexual assault governed by the Korean Ministry of Gender Equality and Family. All data was collected between 2015 and 2016. The present study protocol was reviewed and approved by the Institutional Review Board of Sungshin Women’s University (IRB No. SSWUIRB 2017-004). Only participants who completed written consent forms were included in the study. All participants visited the center within an average of 4 days after trauma and completed questionnaires after their initial visit.
Measures
Insomnia Severity Index
The Insomnia Severity Index (ISI) is a 7-item questionnaire that evaluates insomnia symptom severity [10]. Each of the ISI items are scored on a 5-point Likert scale ranging from 0 to 4. A total score is calculated by summing up the whole items, ranging from 0 to 28, with higher scores indicating greater insomnia severity. According to Cho et al. [11], a cut-off score of 15 was suggested for the Korean ISI, and this study also classified insomnia groups based on this score. Internal consistency of this questionnaire was 0.90 in this sample.
PTSD Symptom Scale-Self Report
The PTSD Symptom Scale-Self Report (PSS-SR) is a 17-item self-report questionnaire that assesses PTSD symptoms, including re-experiencing, avoidance, and hyper-arousal symptoms [12]. Each of the items is rated on a 4-point Likert scale. The total PSS-SR score is the sum of all items, with higher scores indicating PTSD severity. The PSS-SR used in this study was translated as Hong and Park [13]. Internal consistency of this questionnaire was 0.93 in this sample.
Trauma-Related Guilt Inventory
The Trauma-Related Guilt Inventory (TRGI) is a 32 item questionnaire evaluating guilt associated with a particular trauma event [14]. Each of the items is measured on a 5-point Likert scale, ranging from 0 to 4. The TRGI consists of three subscales: global guilt, distress and guilt cognitions. Guilt cognitions can further be divided into Hindsight-Bias/Responsibility (e.g., I was responsible for causing what happened), Wrongdoing (e.g., I had some thoughts or beliefs that I should not have had), and Lack of Justification (e.g., I had good reasons for doing what I did) subscales. The higher the average score of each item, the higher the perception of guilt in the trauma. In this study, we used the TRGI developed by Kubany et al. [14]. Internal consistency of this questionnaire was 0.82 in this sample.
Beck Depression Inventory
The Beck Depression Inventory is a 21-item self-report questionnaire measuring severity of depressive symptoms [15]. Each item is rated on a 4-point Likert scale of 0 to 3, with totals ranging from 0 to 63. Higher scores reflect more depressive symptoms. In this study, we used the Korean version of the Beck Depression Scale, which was translated by Lee and Song [16]. Internal consistency of this questionnaire was 0.93 in this sample.
Statistical Analyses
Correlational analyses were conducted using Pearson’s correlation coefficient between insomnia symptoms, PTSD symptom and trauma-related guilt. All participants were divided into two groups based on their ISI scores. Analysis of covariance (ANCOVA) was conducted to analyze differences in trauma-related guilt between the two groups after controlling for depression. Test of normality in the TRGI score were conducted using the Shapiro-Wilk test. Assuming normality, the ANCOVA would be performed. TRGI distress data is not normal, a nonparametric approach (i.e., ranked ANCOVA) would be performed. All statistical analyses were conducted using SPSS 21.0 (IBM Corp., Armonk, NY, USA).
RESULTS
Demographic Information
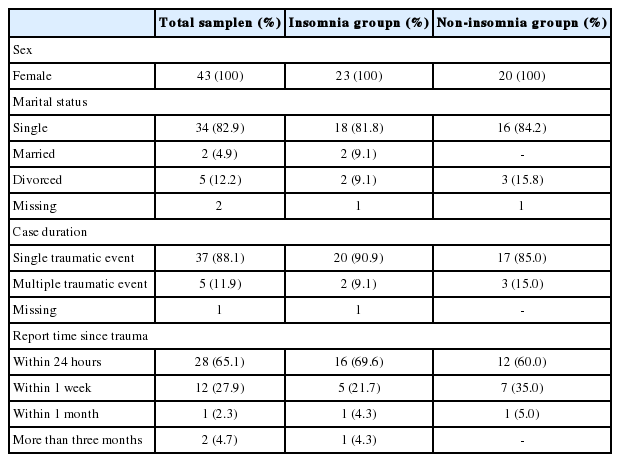
Demographic characteristics of the participants are shown in Table 1. All participants were females who were victims of sexual assault (mean age 26.56 ± 7.81), with 88.1% (n = 37) of the sample experiencing a single traumatic event and 11.9% (n = 5) experiencing multiple traumatic events. In our sample, there were 23 patients in the insomnia group and 20 patients in the non-insomnia group. The average ISI score of the insomnia group was 21.39 (± 3.86) and the non-insomnia group was 11.05 (± 3.38). Differences in PTSD symptom between the Insomnia group and non-Insomnia group can be found in Table 2. Based on the group difference test result about the severity of the insomnia, significant group difference was found in avoidance (p < 0.006), intrusion (p < 0.003), and hyperarousal (p < 0.012) the subfactors of PSS symptoms, respectively. However, both groups reported avoidance as the most severe symptoms compared to other symptoms.
Association between Insomnia Symptom, PTSD Symptom and Trauma-Related Guilt
ISI scores were significantly positively associated with PSS scores (r = 0.620, p < 0.01) and the distress subscale of the TGRI (r = 0.488, p < 0.01). ISI scores were also negatively associated with guilt cognitions (r = -0.423, p < 0.01). Results indicate that higher severity of insomnia was associated with more PTSD symptoms, more trauma-related distress, and less perception of trauma-related guilt (Table 3 for correlates).
Trauma-Related Guilt Based on Insomnia Severity
The insomnia group scored significantly lower in overall guilt cognitions [F(2, 39) = 16.760, p < 0.001] and significantly higher in distress [F(2, 39) = 11.599, p = 0.001] than the non-insomnia group after controlling for depression. Among the subscales of guilt cognitions, hindsight-bias/responsibility was significantly lower in the insomnia group [F(2, 39) = 18.100, p < 0.001]. Results are shown in Table 4.
DISCUSSION
The current study investigated trauma-related guilt in female victims of sexual violence based on insomnia severity. While PTSD patients experience sleep disturbance and psychological changes after trauma [17], trauma-related guilt in this population is an area that has yet to be investigated in depth. In this respect, this is the first study to examine trauma-related guilt in PTSD patients with sexual trauma in relation to sleep disturbance. The main results of our study indicate that individuals with higher levels of insomnia symptoms report higher distress and lower guilt cognition after controlling for depression.
Sleep Disturbance in PTSD Patients with Sexual Violence History
In our sample, 53.7% reported having clinical levels of insomnia, with those in the high risk group reporting particular difficulty with sleep initiation and maintenance. This is consistent with past studies that have found that individuals with sexual abuse history had longer sleep latencies and frequent nightmares than those without abuse history Steine et al. [5]. According to another previous study, 63% of female who experienced sexual assault and had PTSD complained of pain by nightmares and experienced difficulty maintaining sleep due to nightmares [18]. PTSD patients may also experience fear of sleep due to trauma-related nightmares or dreams, thereby experiencing difficulty with sleep initiation and maintenance [19]. Additionally, for people with sexual violence history, the bedroom may be perceived as threatening because sexual abuse may have occurred in the bedroom, thus making it a salient stimulus. This can lead the patient to perceive additional threats to safety and protection, which may subsequently exacerbate sleep disturbance [20].
PTSD patients experiencing sleep disorders can also be explained from a biological perspective. Individuals who have experienced a shocking event have fight-or-flight response to protect themselves. However, even after the actual risk has disappeared, the fight-or-flight response may remain and cause over-activation of the sympathetic nervous system, resulting in heightened arousal level. In addition to an overactive autonomic nervous system, the hypothalamus-pituitary-adrenal axis may be activated when the patient has been exposed to multiple traumas. This may lead to frequent awakenings that interfere with normal sleeping, and attenuates the recovery effect of sleep, resulting in insomnia [21]. Thus, females with sexual trauma may be more vulnerable to insomnia than PTSD patients with other types of trauma.
Lower Guilt Cognition Associated with Higher Insomnia Risk
In our study, participants who were at higher risk for insomnia reported higher distress and lower guilt cognition compared to individuals who had lower insomnia risk. This result supports the findings that sleep in PTSD patients of sexual violence is associated with trauma-related cognitive and emotional factors [17,22]. Individuals exposed to an unexpectedly shocking event require processing to cope with the event. Individuals exposed to trauma experience inconsistencies in existing memory structures due to negative emotional information related to traumatic experiences. One way trauma victims try to integrate the new traumatic experience with existing cognitive systems is by recalling traumatic events over time. During this process, the failure to integrate trauma-related information causes symptoms of PTSD [23]. Sleep in PTSD patients plays an important role in the integration and processing of traumatic events [24]. In particular, sleep is associated with the regulation of cognitive and emotional brain processes, and abnormalities in sleep function are reported to be difficulties in cognitive and emotional processing [25,26]. Importantly, high levels of insomnia symptoms were associated with low guilt cognition. This result speculates that low guilt cognition may reflect active avoidance of processing trauma-related cues in this population. This was also supported in our study, as the insomnia group reported highest on avoidance compared to other PTSD symptoms.
The results of having low guilt cognition in insomnia patients are somewhat inconsistent with previous studies. This may be reflective of previous studies investigating the role of guilt without differentiating it from shame, which is a similar emotion. In previous studies, most studies have reported a positive association between guilt and PTSD symptoms. But in some studies, when controlling for the effects of shame, PTSD symptom and guilt were found to be negatively associated [27–29]. Shame is frequently activated simultaneously with guilt after trauma, and both shame and guilt are similar in that they are associated with evaluating feelings related to the self. However, in contrast to guilt, shame involves an assessment of the overall self, such as “I am a bad person” [28,30]. As in previous studies, our results suggest that guilt can serve as a protective factor for individuals in PTSD development [30–32]. In particular, it is noteworthy that the absence of experience of trauma-related guilt plays an important role in trauma-related sleep disorders. According to a study by van Minnen et al. [33], individuals with little or no guilt had no statistical room for improvement in PTSD symptoms, and individuals who actually have extreme initial scores tend to be maintained or increased after treatment. In other words, these results suggest that it may be more adaptive to face and accept negative cognitions and emotions such as guilt that are related to the trauma experience. Especially, focusing on the perception of dysfunctional behavior will provide an opportunity to search for adaptive negative emotions.
In our study, we studied trauma-related guilt, which was distinguished from shame and the sub-factors of guilt was examined in detail. Our results reported significantly lower guilt in the insomnia group. Especially, it showed significantly low score in ‘Hindsight-Bias/Responsibility’ in individuals with insomnia. Hindsight-Bias/Responsibility is a guilt-related cognition that reflects how much an individual believes they possess knowledge of the outcome of an event and predict its outcome. For example, a sexual assault victim with high hindsight bias/responsibility would believe that they should have “known something goes wrong” or “directed to the other direction,” and they feel responsible for not revealing the past abuse. This may lead to excessive self-blame by believing that trauma survivors were overburdened by trauma events or related negative consequences and were able to avoid trauma events [7,34]. If a trauma survivor falsely believes he or she had pre-outcome knowledge that would have enabled him or her to change the course of trauma events, it follows logically that they “chose” not to prevent the event and thereby is responsible to some extent for having caused the event [7]. According to Ianoff-Bulman [35], it has been proposed that the protective factor can be a function of the type of self-blame. Self-blame for specific behaviors that change the cause of traumatic experiences into controllable or modifiable aspects such as specific behaviors can be more adaptive compared to characterological self-blame attributed to uncontrollable aspects such as one’s personality. In a previous study of self-blame, behavioral self-blame in trauma events showed that event-related pain decreased over time [36], and in a study of victims of sexual assault, a group with high self-criticism behavior was found to be adaptive in coping with trauma events [37]. More specifically, the post-confirmation bias is high when you agree with the question “I could have prevented what happened,” “I blame myself for something I did, thought, or felt.” Higher scores on these questions reflect more negative the behavior that failed, which may facilitate an active process in restructuring the existing cognitive system and subsequently help recovery. According to some studies, higher guilt tendency after the negative experience was more closely associated with the degree that a respondent accepts his or her experience as it is [29]. Considering this point, sleep can be an important factor in dealing with traumatic events. Especially, when females who experience sexual violence display lower guilt, it may lead to avoidance of evaluating and exploring the cause of the event and moving past blaming themselves for controllable or modifiable aspects of the traumatic event.
Clinical Implications
The relationship between insomnia and trauma-related guilt in females with sexual violence has several important clinical implications. Previous studies have shown that PTSD patients with insomnia have worse clinical outcomes than patients who have PTSD without insomnia. In addition, patients with previous sexual violence experiences reported significantly more than those who experienced other trauma. From a clinical point of view, our results suggest that female with a history of sexual violence may be more vulnerable to insomnia and that access to sleep problems is important in treating them. Previous studies have shown that patients with PTSD frequently have negative mood states, such as depression, and that the effects of these moods can have a significant impact on PTSD-related symptoms [38,39]. This study is meaningful in that it explains the relationship between two concepts independent of the control of depression by statistical methods. Many PTSD psychotherapy studies have shown that facing and accepting emotions associated with trauma events was effective in alleviating PTSD symptoms [33,40]. Trauma-related guilt is a form of emotion that includes self-assessment of traumatic experiences and is often mixed with shame. Our results suggest that assessing traumatic guilt in the context of sleep disturbance in PTSD patients, especially females with sexual trauma, may be helpful in the treatment of women who experience sexual abuse. If the trauma is perceived to be a violation of a specific rule, it will be a strategy to reduce the individual suffering from trauma, leading to a process of activating a fundamental belief in oneself or confirming their experience. In this respect, future studies should focus on whether providing sleep specific treatment in addition to traditional psychotherapy may help improve sleep, and subsequently affect trauma-related guilt and activate the recovery process.
Limitations
The limitations of this study and suggestions for future research are as follows. First, this study had a small sample size. Additional studies with larger sample sizes are needed to further elucidate the role of sleep in the process of coping with trauma. Second, the unity of the initial assessment period after the incident was insufficient. Most of the initial assessments were made within average of 6 days after their initial visit, but the unity of the period from one month to three months after the occurrence of the incident was insufficient. Therefore, future studies need to consider the evaluation period after the incident. Third, in this study, TRGI was used to measure Trauma-Related Guilt. TRGI includes perceived wrong-doing, responsibility and self-blame that may be particularly relevant to the cognitive, affective, and behavioral components of guilt. This tool is reported to be an excellent measure of the guilt properties, but it is difficult to completely exclude the possibility of also measuring shame. In future studies, it is necessary to distinguish between guilt and shame, including measures of shame. Also, because this study is a retrospective study, it did not include a questionnaire to evaluate the coping strategy or post-traumatic perception in advance. In future studies, it is necessary to verify the cognitive factors after trauma, whether using low avoidance coping strategies or low guilt feelings. Fourth, the present study has limitations in revealing the causal relationship in the nature of the study because it was a cross-sectional study. Therefore, it will be necessary in future studies to investigate the path of insomnia symptoms and trauma-related guilt level of women who have experienced sexual violence by supplementing these limitations. Finally, although this study suggests that guilt may serve as a protective factor, there are limits to understanding the impact of long-term trauma-related guilt. Future research should investigate the longitudinal effects of guilt on the recovery of PTSD symptoms.
Conclusion
Results from the current study indicated the association between insomnia and trauma-related guilt in females with sexual violence history. Our findings suggest that sleep disturbance in these individuals may be associated with lower guilt, which may prevent these individuals from actively processing their trauma experience. These results imply that it will be important for clinicians to assess and be mindful of trauma-related guilt, especially differentiated from shame. Furthermore, future studies should focus on the role of guilt and develop and incorporate specific interventions that can actively process guilt in this population.
Notes
Conflicts of Interest
The authors have no financial conflicts of interest.
Authors’ Contribution
Study design: Han SR, Chang HY, Suh SY. Data collection: Chung YK, Kim MR, Lee HB, Kim YJ, Chang HY. Data analysis: Han SR. Interpretation of results: Han SR, Chang HY, Suh SY. Preparation of the manuscript: Han SR, Lee HB, Kim YJ, Chang HY, Suh SY. Critical review of the manuscript: Chung YK, Kim MR. Writing—original draft: Han SR. Writing— review & editing: Chang HY, Suh SY.