Cheyne-Stokes breathing (CSB) is a form of periodic breathing with at least three consecutive events starting with central apnea/hypopnea, followed by crescendo-decrescendo breathing (cycle length > 40 seconds), and at least 2-hour monitoring should reveal central apnea index > 5 events/hour [1]. The most common cause of CSB is heart failure, in which the cardiac output decreases, circulation delay between lungs and chemoreceptors increases, and chemoreflex instability (loop gain) increases [2]. A patient with heart failure is at high risk of obstructive sleep apnea [1]. Here, we report the case of a patient with heart failure and multiple cardiovascular risks who exhibited typical CSB during non-rapid eye movement (non-REM) sleep and then changed to atypical CSB during REM sleep, and discuss the breathing mechanisms.
A 72-year-old man presented with snoring, apnea, and periodic breathing. He was 169 cm tall and weighed 65 kg. He had taken medication for hypertension, dyslipidemia, heart failure, diabetes mellitus, and atrial fibrillation, and he had a history of coronary angioplasty. He had consumed one bottle of alcoholic beverage in one week. He was hospitalized with multiple embolic infarctions in the left middle cerebral artery territory at the time of polysomnography (PSG). Sleep and REM latency was 1.5 minutes and 13 minutes, respectively. Total sleep time was 369 minutes. Sleep efficiency was 76.1%. He slept in a supine position during his total sleep time. The total apnea-hypopnea index was 55 events/hour (central apnea index 45.2 events/hour, mixed apnea index 7.4 events/hour, and obstructive apnea index, 2.4 events/hour). The arousal index was 28.9 events/hour.
The PSG showed typical CSB during non-REM sleep. The mean cycle length was 80.5 ± 3.5 seconds during non-REM sleep. Periodic cyclic breathing persisted all night; however, a typical CSB pattern starting with central apnea changed to an atypical pattern starting with mixed apnea during REM sleep (cycle length, 92.2 ± 7.1 seconds) (Fig. 1). These changes occurred because of stabilization of chemoreflex instability (shortened length of central apnea: 44.2 ± 3.7 during non-REM sleep vs. 39.9 ± 2.6 during REM sleep, p < 0.001) and earlier regainment of respiratory effort) and increased upper airway collapsibility.
Upper airway collapsibility increases during REM sleep as activities of upper airway dilator muscles decrease [3]. However, the chemoreflex instability weakens during REM sleep, indicating a more stable ventilatory control; thus CSB diminishes or disappears during REM sleep [4]. In adults, mixed apnea is characterized by a combination of central and obstructive apnea, which means no initial respiratory effort and airflow, followed by regainment of respiratory effort without airflow. The underlying pathophysiology of mixed apnea comprises an increased chemoreflex instability and upper airway collapsibility. This peculiar case highlights the sleep stage- dependent interactions between chemoreflex instability and upper airway collapsibility in CSB.
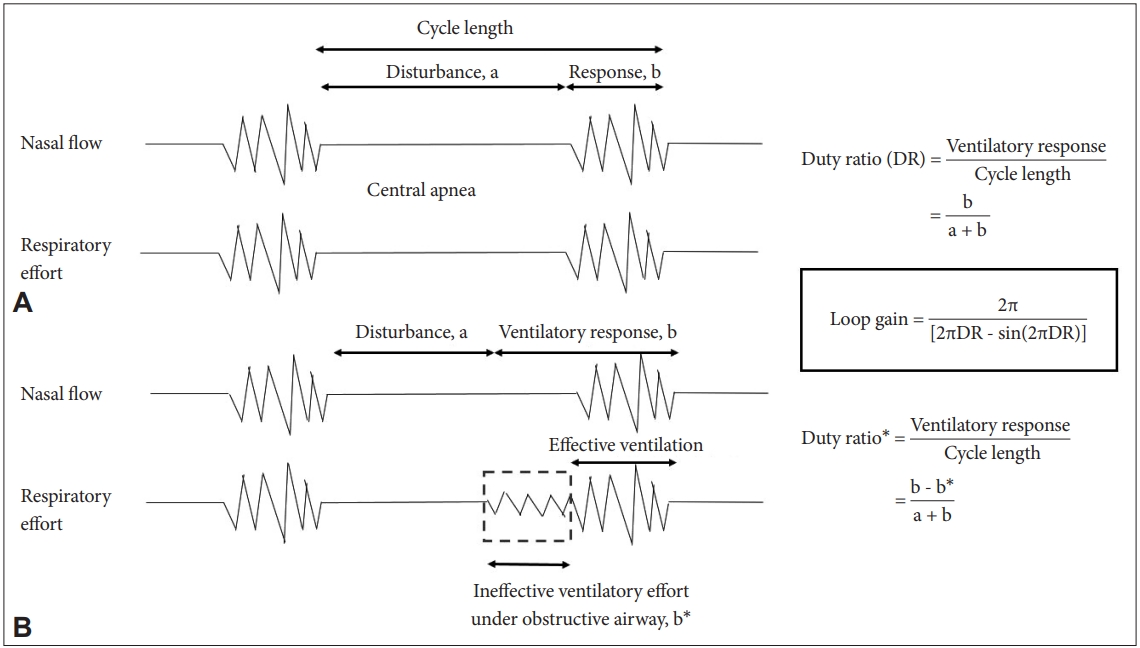
Breathing mechanisms can be proven by the estimated loop gain with PSG data [4,5]. The duty ratio can be defined as ventilation length divided by cycle length. The cycle length is defined as the duration of apnea length plus ventilation length. Loop gain can be estimated as 2π/[2π∙duty ratio - sin(2π∙duty ratio)] (Fig. 2) [5]. Technically, while dealing with mixed apnea, it should be noted that central apnea is included as apnea length, but obstructive apnea is included as a part of ventilation length because an ineffective ventilatory effort is presented under an obstructed airway. Then loop gain during non-REM (N1 and N2 in this case) and REM sleep can be calculated. Mean loop gain during non-REM and REM sleep were calculated as 2.55 ± 0.47 and 1.62 ± 0.20, respectively (p < 0.001). Although loop gain decreased during REM sleep, it remained above 1; thus periodic CSB persisted throughout the night.