AbstractBackground and Objective We tested the psychometric properties of the Stress and Anxiety to Viral Epidemics-9 (SAVE-9) scale among healthcare workers who experienced patients’ deaths.
Methods From June 2nd to 10th, 2022, an anonymous, online survey was administered to medical doctors and nursing professionals who witnessed the deaths of patients they cared for during the last two years. Participants demographic characteristics and responses to the SAVE-9, Generalized Anxiety Disorder-7 (GAD-7), Patient Health Questionnaire-9 (PHQ-9), and Insomnia Severity Index (ISI) were collected.
Results A total of 267 responses were collected in this survey. The two-factor model of the SAVE-9 fits well among healthcare workers who witnessed patients’ death (CFI = 1.000, GFI = 0.996, RMSEA = 0.000, RSMR = 0.040). The SAVE-9 scale showed good reliability of internal consistency and convergent validity with the GAD-7 (r = 0.429, p = 0.001), PHQ-9 score (r = 0.414, p = 0.001), and ISI (r = 0.368, p = 0.001).
INTRODUCTIONCoronavirus disease 2019 (COVID-19) was first identified from an outbreak in Wuhan, China, in December 2019. The novel virus has infected more than 612 million persons worldwide and killed more than 6 million patients and unfortunately, these numbers keep on increasing [1]. This crisis has added a huge burden on healthcare workers who had the responsibility to make the right diagnosis, give the treatment and the ultimate care of patients affected by COVID-19. At some point in this pandemic, healthcare workers spent an average of 16 hours per day taking care of infected patients [2]. Furthermore, the fear of being infected, or transmitting the disease to their loved ones, and even working with new and changing protocols, and even keeping personal protective equipment made the workload harder and harder [3].
Another major impact of this crisis on healthcare workers is the effect of patients’ death on the mental health of the physicians themselves. Death of patients is an unavoidable experience in the journey of a physician, and despite this widespread phenomenon, studies conducted on the mental health of healthcare workers and especially during COVID-19 crisis are very limited. The literature affirms the presence of grief reactions among healthcare workers in response to patient death [4]. This stressful event can go beyond that so it’s been linked to professional burnout and even considered as a risk factor for getting psychiatric disorders [5]. Witnessing patient death in COVID-19 pandemic was reported to be a risk factor for mental health such as post-traumatic stress [6], among healthcare workers. Some studies focused on the reaction of physicians from specific specialties such as surgeons and pediatric oncologists toward death of their patients, and in both this experience found to be related to psychological burden or impact with a wide range of manifestations [7,8].
Recently, we have developed a viral anxiety rating scale specific for the healthcare workers, the Stress and Anxiety to Viral Epidemics-9 items (SAVE-9) scale [9]. The SAVE-9 scale was validated in Korean and various languages [10-15]. However, there was no previous study which was conducted among healthcare workers who experienced patients’ death whom they took care of. Since facing patients’ death is a desperately stressful experience to healthcare workers, assessing work-related stress or viral anxiety is important. We aimed in this study to explore the reliability and validity of the SAVE-9 scale among healthcare workers who experience patients’ death whom they took care of, and explore the relationship of their stress or viral anxiety with their insomnia symptoms or depression.
METHODSParticipants and ProcedureThis online survey study was conducted anonymously in Asan Medical Center during June 2nd–10th, 2022, among medical doctors or nursing professionals who witnessed patients’ death whom they took care of during the last two years. This survey was voluntary, and participants were rewarded with a 5-dollar gift coupon as a reward. The Institutional Review Board of Asan Medical Center approved the study protocol (2022-0740), and it was waived to obtain written informed consent.
Participants were allowed to respond to this survey, if they have witnessed death of patients whom they took care of during the last two years. Participant’s demographic information was collected. As part of the survey, respondents were also asked whether they are caring for infected patients now, whether they have been quarantined, infected, or vaccinated.
Symptom AssessmentStress and Anxiety to Viral Epidemics-9 itemsThe SAVE-9 scale was developed as a tool to assess work-related stress and anxiety of healthcare workers [9]. Previously we reported that nine items on the SAVE-9 were assigned to two factors: SAVE-6 (items 1, 2, 3, 4, 5, and 8 [16]) and SAVE-3 (items 6, 7, and 9-SAVE-3). Items can be scored on a 5-point Likert scale (0: never–4: always), and a higher total score indicates a higher level of work-related stress and viral anxiety.
Generalized Anxiety Disorder-7 itemsA rating scale called Generalized Anxiety Disorder-7 (GAD-7) is used to measure anxiety levels in individuals. Seven items can be rated on 4 point Likert scale (0: not at all–3: nearly every day), and a higher total score indicates a severe degree of anxiety symptoms [17]. In this study, the Korean version of the GAD-7 [18] was used, and Cronbach’s alpha on this sample was 0.900.
Patient Health Questionnaire-9 itemsA rating scale called the Patient Health Questionnaire-9 (PHQ-9) was developed to measure depression. Nine items can be rated on a 4 point Likert scale (0: not at all–3: nearly every day), and a higher total score indicates a severe degree of depression [19]. In this study, the Korean version of the PHQ-9 [18] was used, and Cronbach’s alpha on this sample was 0.901.
Insomnia Severity IndexA rating scale called the Insomnia Severity Index (ISI) was developed to measure insomnia severity [20]. It consists of five items that can be rated on a 6 point Likert scale, with the higher score indicating more severe insomnia symptoms. In this study, the Korean version of the ISI [21] was used, and Cronbach’s alpha on this sample was 0.897.
Statistical AnalysisA confirmatory factor analysis (CFA) was conducted to determine the validity of the two-factor model of the SAVE-9 scale among healthcare workers who witnessed patients’ death. The normality assumption was checked based on skewness and kurtosis within ± 2 [22]. Model fit was examined using standardized root-mean-square residual (SRMR), root-mean-square-error of approximation (RMSEA), comparative fit index (CFI), and Tucker–Lewis index (TLI) values. Multigroup CFA was done to examine the measurement invariance of the scale across sex, having insomnia (ISI ≥ 8) and depression (PHQ-9 ≥ 10). Psychometric properties of the SAVE-9 scale were explored using item response theory (IRT) approach. In the graded response model (GRM), we initially assessed item fits through S- χ2 and its p-values (adjusted for false discovery rate), and values. After that, the slope parameters (α) and threshold parameters (b) were examined, as well as the item characteristic curves of the items were extracted. Besides, scale information curves for the SAVE-9, SAVE-3, SAVE-6, and GAD-7 were extracted to compare which scale function better to assess anxiety. Moreover, IRT reliability was also calculated. Reliability test of the SAVE-9 scale was examined using Cronbach’s alpha. To explore the convergent validity of the SAVE-9 scale and its subscales, we performed Pearson’s correlation analysis with GAD-7, PHQ-9, and ISI scales. The SPSS version 21.0 (IBM Corp., Armonk, NY, USA) and RStudio (R Foundation for Statistical Computing, Vienna, Austria) were utilized for statistical analysis.
RESULTSA total of 267 participants from healthcare workers took part in this study (Table 1). The average age was 31.4 ± 5.4 years (mean ± SD). A total of 78.7% of participants were female and 21.3% were male. Among participants, 63.4% were single and 23.4% were married and had children. In addition, 57.3% of participants were shift-workers. The majority of participants (65.9%) were nurses, while the remaining 34.1% were doctors. There were 15.7% of people reporting a past psychiatric history and 7.1% reported current need help for their psychiatric symptoms. In regards to questions pertaining to COVID-19, 221 (82.8%) were caring for inpatients with COVID-19. Among participants, 264 (98.9%) were fully vaccinated; 155 (58.1%) had been quarantined and 134 (50.2%) had been diagnosed with COVID-19. All participants experienced patients’ death, and 62 (23.2%) reported patients’ death related to the COVID-19.
Factor Structure of SAVE-9 Among Healthcare Workers Who Witnessed Patients’ DeathAll 9 items of the SAVE-9 scale were distributed normally based on the skewness and kurtosis (Table 2). All the items were in the recommended cut-off score. CFA was done for a two-factors model, since the SAVE-9 scale was categorized into Factor I and II in the previous study [9]. We observed a good model fit among healthcare workers who witnessed patients’ death (CFI = 1.000, GFI = 0.996, RMSEA = 0.000, SRMR = 0.040) (Table 3). The multi-group CFAs showed scalar level measurement invariance of the SAVE-9 scale across sex and having insomnia, depression, or generalized anxiety.
Graded Response ModelNonsignificant (≥ 0.05) p-values of the S- χ2 and RMSEA values (< 0.08) indicate that all items belong to the same latent construct (Table 4). In factor I of the SAVE-9 scale (SAVE-6), item 5 has moderate slope compared to other items. Slope parameters (α) for factor I ranged between 1.265 and 3.770 (mean α = 2.335). In terms of threshold coefficients (b) in factor I, item 5 is the most difficult item (Fig. 1A). In factor II, item 9 has moderate slope compared to other two items which have very high slopes. Slope parameters (α) for factor II ranged between 1.299 and 3.279 (mean α = 2.139). In terms of threshold coefficients (b) in factor II, item 9 is the least difficult item compared to others (Fig. 1B). Factor I provides more information than factor II based on scale information curves (Fig. 2). Factor II provides almost the same information as the whole scale. However, GAD-7 provides the highest information compared to factor-I, factor-II, and SAVE-9.
Reliability and Evidence Based on Relations to Other VariablesReliability of internal consistency of the SAVE-9 scale (Cronbach’s alpha = 0.873), and its two factors were shown to be good (factor I, alpha = 0.70 and factor II, alpha = 0.86) (Table 3). For factor I, the item-total correlation ranged between 0.597 and 0.775, while for factor II, it ranged between 0.440 and 0.587. An analysis of convergence validity of SAVE-9 with GAD-7, PHQ-9, and ISI was conducted. Significant correlations were found between the SAVE-9 and the GAD-7 (r = 0.429, p < 0.001), the PHQ-9 (r = 0.414, p < 0.001), and the ISI (r = 0.368, p < 0.001). Additionally, the SAVE 3 and SAVE-6 scales were significantly correlated with the GAD-7, PHQ-9, and ISI scales (Table 5).
DISCUSSIONIn this study, we observed that the SAVE-9 and its two subscales (SAVE-6 and SAVE-3) were valid and reliable tools which can be applied to measure work-related stress and viral anxiety of healthcare workers who witnessed death of patients whom they took care for. The CFA showed good model fits for the two factor (SAVE-6 and SAVE-3) model of the SAVE-9 scale among this sample. The SAVE-9 and its two subscales showed good reliability, and showed good convergent validity with rating scales of depression, generalized anxiety, or insomnia.
Coronavirus outbreak has caused a huge burden on healthcare workers and increased time spent caring for infected patients [23]. As the fear of infection or transmission of the disease increased, the workload became more and more difficult. Additionally, the death of the patients caused distress on the mental health of the healthcare workers. This could have caused burnout or even contributed to the development of psychiatric disorders. Although only 23.2% of those who died from coronavirus in this study, whether a patient’s death is directly attributable to the virus is not of great importance in a pandemic situation. It is very important to evaluate how corona-related job stress and anxiety affects medical personnel during a pandemic. Therefore, it is important to explore the usefulness of the SAVE-9 scale among healthcare workers who witnessed the death of patients who they took care for.
In GRM, item 5 of factor I and item 9 of factor II have moderate slope parameters (α), but item 5 is the most difficult item among factor I and item 9 is the least difficult item among factor II in relation to threshold coefficients (b). The usefulness of item 5 (Are you worried that others might avoid you even after the infection risk has been minimized?) is one of the issues in the SAVE-9. When COVID-19 first spread, healthcare workers faced the worry that they were contagious to their neighbors who live adjacent to them. However, the usefulness of this item is now low in this pandemic era when all the people can be infected. We observed that item 9 (Do you think that your colleagues would have more work to do due to your absence from a possible quarantine and might blame you?) is the least difficult item among factor II. We can expect that healthcare workers felt depressed or frustrated when they faced patients’ death. They should have wanted to have a rest in this situation, but, at the same time, they might have worried about their colleagues’ workload in their absence. It might influence the results.
Scale information curves showed that the SAVE-9 and SAVE-6 provide similar information, and these have more information than the SAVE-3 scale. The similar information between the SAVE-9 and SAVE-6 shows us that we can apply the SAVE-6 scale rather than the full scale of the SAVE-9 when we assess healthcare workers’ viral anxiety in this pandemic. In our previous study on healthcare workers in Spain [24], we observed that it was feasible to apply the SAVE-6 scale to them while maintaining some of its “specificity to the viral epidemic,” despite losing some of its “specificity to healthcare workers.”
The GAD-7 provides the highest information compared to factor-I, factor-II, and SAVE-9. The SAVE-9 scale was developed specifically to identify healthcare workers who would benefit from psychological support [9], and we observed that 22.8% of workers, who were not screened by the GAD-7, were found as having stress and anxiety in response to COVID-19. The result of this study shows that the GAD-7 is informative similar to our previous study [25], but the GAD-7 scale cannot assess viral anxiety specifically in response to viral epidemic but nonspecific generalized anxiety.
There are several limitations in this study. First, the small sample size of this study cannot be generalizable to the whole healthcare workers population. We collected just 91 of 1759 medical doctors (5.2%) and 176 of 4526 nursing professionals (4.1%) in Asan Medical center. Small sample size may increase type II error. However, we recruited participants who witnessed the death of patients whom they took care of, and it may be one of the strengths of this study. Second, an online anonymous survey was done rather than face-to-face interview in this study. In this pandemic, online surveys are beneficial to prevent the viral transmission. Furthermore, the issue of witnessing patients’ death may be a sensitive issue for healthcare workers, and participants preferred anonymous online surveys compared to face-to-face interviews. Third, 62 (23.2%) of participants witnessed patients’ death due to COVID-19 pandemic, though all participants witnessed patients death regardless of COVID-19. Despite the fact that we did not intend to collect the healthcare workers who witnessed patients’ death due to COVID-19 infection, a low proportion of COVID-19 related deaths may be considered in the interpretation of this study. On the other hand, it is not often clear whether the patient’s death may come from COVID-19 infection or not in the clinical field.
In conclusion, we observed that SAVE-9 and its subscales can be applied to healthcare workers who witness patients’ death in COVID-19 pandemic with a good reliability and validity. Since witnessing a patient’s death is absolutely a great traumatic experience to healthcare workers, we hope that this SAVE-9 scale can be appropriately used to assess viral anxiety of healthcare workers.
NOTESAvailability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
ACKNOWLEDGEMENTSWe would like to thank Dr. Seockhoon Chung, Professor in the Department of Psychiatry, University of Ulsan College of Medicine for a wonderful discussion about this study.
REFERENCES1. World Health Organization. WHO coronavirus (COVID-19) dashboard [cited 2021 Sep 9]. Available from: https://covid19.who.int/.
2. Saragih ID, Tonapa SI, Saragih IS, Advani S, Batubara SO, Suarilah I, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud 2021;121:104002.
3. Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiovasc Care 2020;9:241-7.
4. Sansone RA, Sansone LA. Physician grief with patient death. Innov Clin Neurosci 2012;9:22-6.
5. Redinbaugh EM, Sullivan AM, Block SD, Gadmer NM, Lakoma M, Mitchell AM, et al. Doctors’ emotional reactions to recent death of a patient: cross sectional study of hospital doctors. BMJ 2003;327:185.
6. Mosheva M, Gross R, Hertz-Palmor N, Hasson-Ohayon I, Kaplan R, Cleper R, et al. The association between witnessing patient death and mental health outcomes in frontline COVID-19 healthcare workers. Depress Anxiety 2021;38:468-79.
7. Joliat GR, Demartines N, Uldry E. Systematic review of the impact of patient death on surgeons. Br J Surg 2019;106:1429-32.
8. Granek L, Bartels U, Scheinemann K, Labrecque M, Barrera M. Grief reactions and impact of patient death on pediatric oncologists. Pediatr Blood Cancer 2015;62:134-42.
9. Chung S, Kim HJ, Ahn MH, Yeo S, Lee J, Kim K, et al. Development of the stress and anxiety to viral epidemics-9 (SAVE-9) scale for assessing work-related stress and anxiety in healthcare workers in response to viral epidemics. J Korean Med Sci 2021;36:e319.
10. Uzun N, Akça ÖF, Bilgiç A, Chung S. The validity and reliability of the stress and anxiety to viral epidemics-9 items scale in Turkish health care professionals. J Community Psychol 2022;50:797-805.
11. Mosolova E, Chung S, Sosin D, Mosolov S. Stress and anxiety among healthcare workers associated with COVID-19 pandemic in Russia. Psychiatr Danub 2020;32:549-56.
12. Tavormina G, Tavormina MGM, Franza F, Aldi G, Amici P, Amorosi M, et al. A new rating scale (SAVE-9) to demonstrate the stress and anxiety in the healthcare workers during the COVID-19 viral epidemic. Psychiatr Danub 2020;32(Suppl 1):5-9.
13. König J, Chung S, Ertl V, Doering BK, Comtesse H, Unterhitzenberger J, et al. The German translation of the stress and anxiety to viral epidemics-9 (SAVE-9) scale: results from healthcare workers during the second wave of COVID-19. Int J Environ Res Public Health 2021;18:9377.
14. Okajima I, Chung S, Suh S. Validation of the Japanese version of stress and anxiety to viral epidemics-9 (SAVE-9) and relationship among stress, insomnia, anxiety, and depression in healthcare workers exposed to coronavirus disease 2019. Sleep Med 2021;84:397-402.
15. Wasimin FS, Thum SCC, Tseu MWL, Kamu A, Ho CM, Pang NTP, et al. Adaptation and validation of the Malay version of the SAVE-9 viral epidemic anxiety scale for healthcare workers. Int J Environ Res Public Health 2022;19:10673.
16. Chung S, Ahn MH, Lee S, Kang S, Suh S, Shin YW. The stress and anxiety to viral epidemics-6 items (SAVE-6) scale: a new instrument for assessing the anxiety response of general population to the viral epidemic during the COVID-19 pandemic. Front Psychol 2021;12:669606.
17. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7.
19. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13.
20. Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011;34:601-8.
21. Cho YW, Song ML, Morin CM. Validation of a Korean version of the insomnia severity index. J Clin Neurol 2014;10:210-5.
22. Gravetter F, Wallnau L. Essentials of statistics for the behavioral sciences. 8th ed. Belmont, CA: Wadsworth 2014.
23. Ahn MH, Shin YW, Suh S, Kim JH, Kim HJ, Lee KU, et al. High work-related stress and anxiety as a response to COVID-19 among health care workers in South Korea: cross-sectional online survey study. JMIR Public Health Surveill 2021;7:e25489.
Fig. 1.Threshold characteristics curves of factor I (SAVE-6) (A) and factor II (SAVE-3) (B). SAVE, Stress and Anxiety to Viral Epidemic. 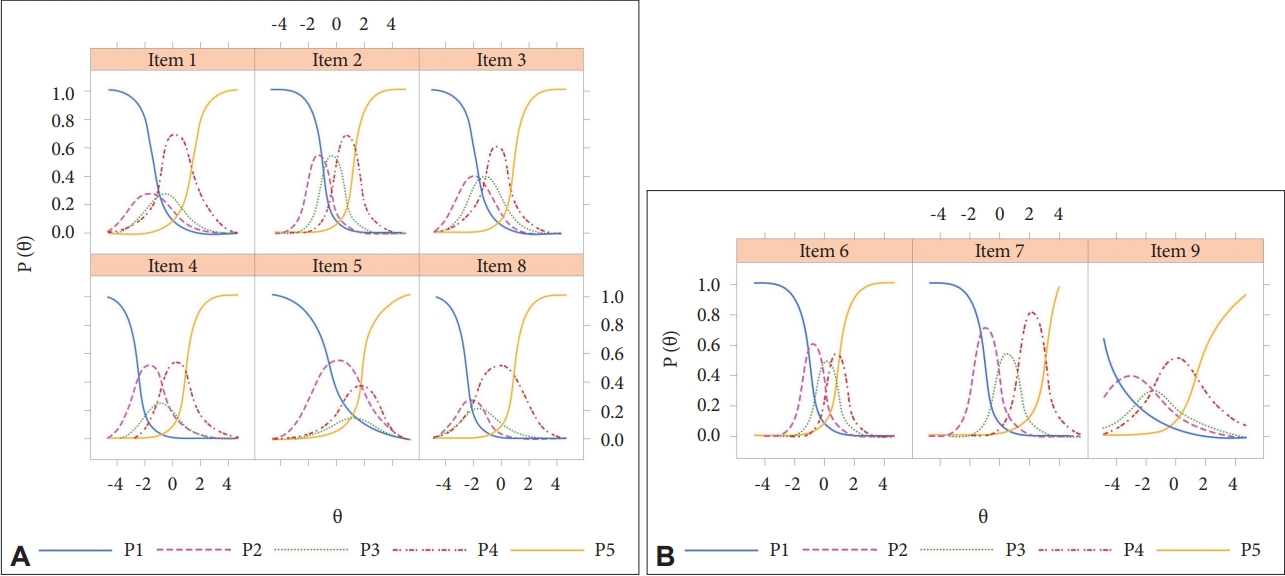
Fig. 2.Scale information curve. GAD-7, Generalized Anxiety Disorder-7 items; SAVE, Stress and Anxiety to Viral Epidemic. 
Table 1.Clinical characteristics of participants (n = 267)
Table 2.Item properties of the SAVE-9 scale among healthcare workers who witnessed the death of patients whom they cared for Table 3.Scale level psychometric properties of the SAVE-9 scale among healthcare workers who witnessed the death of patients whom they cared for Table 4.Item fit, and slope and threshold parameters of the SAVE-9 scale among healthcare workers who witnessed the death of patients whom they cared for Table 5.Pearson correlation coefficients of each variables in all participants (n = 267)
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||