AbstractBackground and Objective Several studies have raised questions about determining the diagnosis of the narcolepsy using multiple sleep latency test (MSLT). In this study, we investigated the diagnostic change in narcolepsy type 1 (NT1) and narcolepsy type 2 (NT2) using MSLT with long-term interval.
Methods In this retrospective study, the demographic characteristics, polysomnography (PSG), and MSLT parameters were compared at the baseline between the NT1 and NT 2 patients. Then, MSLT re-tests were conducted with a mean follow-up of 8.48 years in patients with NT 1 and 7.05 years with NT 2.
Results Seventy-four patients (58 with NT1 and 16 with NT2) were investigated in this study. At the baseline, demographic data showed a larger body mass index value, more sleep paralysis, and hypnogogic hallucination in NT 1 compared to NT 2. Also, at baseline MSLT, shorter mean sleep latency and higher number of sleep onset rapid eye movement periods (SOREMPs) were observed in the NT 1 than those of the NT 2. On follow-up MSLT, 6.9% (n = 4) patients with NT1 and 50% (n = 8) patients with NT2 did not satisfy the previous diagnosis. Furthermore, in all the groups who had the change in repeated-MSLT, the groups with less than 2 SOREMPs observed to be accompanied by negative MSL at follow-up.
INTRODUCTIONCentral hypersomnolence disorders are excessive daytime sleepiness in the absence of nocturnal sleep pathology or insufficient sleep [1-5], including narcolepsy with or without cataplexy and idiopathic hypersomnia (IH) [6]. Cataplexy is a symptom mainly caused by hypocretin/orexin deficiency and is an essential criterion for classifying narcolepsy types. In this regard, according to the International Classification of Sleep Disorder (3rd edition, 2014), narcolepsy type 1 (NT 1) has cataplexy, abnormally low hypocretin in the cerebrospinal fluid (CSF), and two or more sleep onset rapid eye movement periods (SOREMPs) and the presence of abnormal sleep latency. Narcolepsy type 2 (NT 2) has no cataplexy with normal CSF hypocretin but shows similar multiple sleep latency test (MSLT) results to narcolepsy type 1. Furthermore, IH has no elastic seizures, normal CSF hypocretin, and no SOREMP, but abnormal sleep latency on MSLT [7].
Since measuring the concentration of hypocretin is an invasive and expensive process with a high risk of infection, the diagnosis of narcolepsy has been mainly based on MSLT [8]. However, many studies have raised numerous questions about the validity of MSLT. In one study, MSLT was performed again after a mean of 4.2 years for a total of 36 patients diagnosed with type 2 narcolepsy and IH [6]. Notably, the proportion of diagnosis change was observed to be 53%, specifically 10 out of 15 patients with type 2, and 6 out of 14 patients with IH [6]. In contrast, Um et al. [9] reported that different MSLT results occurred only for 2 out of 48 patients diagnosed as NT1 patients in the follow-up MSLT from the initial, most patients satisfying the NT 1 criteria as well. At this moment, it should be noted that these researches had an intrinsic limitation that the number of patients was relatively small.
There have not been many studies on MSLT validity in narcolepsy patients with more than 5 years of follow-up in Korean sleep centers. In this study, we intended to analyze the differences in follow up MSLT parameters of NT1 and NT2, along with their baseline clinical disparities.
We hypothesized that there will be differences in baseline and follow up MSLT between NT1 and NT2 group. Moreover, we hypothesized that the diagnostic changes and clinical course will be disparate between the two groups.
METHODSParticipants and Patient EvaluationAmong the patients who visited the sleep center of the St. Vincent’s Hospital, College of Medicine, Catholic University of Korea for excessive daytime sleepiness between 2001 through 2017, we retrospectively reviewed the medical records of 74 patients who underwent MSLT twice or more within the follow up period of 5 years. Narcolepsy is a rare disease, and patients get financial support with the help of the national health insurance. Re-registration is necessary every 5 years, and updated MSLT result is required each time. As baseline, all the participants were drug-naïve, and a diagnosis of narcolepsy type 1 or narcolepsy type 2 was made using the International Classification of Sleep Disorders-Second Edition [1] and the International Classification of Sleep Disorders-Third Edition (ICSD-3) criteria [2]. Because hypocretin detection in the CSF could not be performed, NT1 was diagnosed when there was clear cataplexy or a history of cataplexy. This study was conducted after approval by the Institutional Review Board of St. Vincent’s Hospital, the Catholic University of Korea. The survey protocol was approved by the Korea Centers for Disease Control and Prevention Institutional Review Board (IRB No. VC21RASI0104).
Statistical AnalysisWe analyzed 74 patients who were diagnosed with either narcolepsy type 1 or narcolepsy type 2 at first with the baseline demographic data and sleep parameters of MSLT, and nocturnal polysomnography (PSG). Then, at the second visit for follow-up, the sleep parameters of MSLT were compared between the two groups.
In the first dataset, the baseline demographic data and sleep parameters of MSLT, and nocturnal PSG were compared between the NT 1 and NT 2 groups. The chi-square test was used for the categorical variable and the independent t-test was used for the continuous variable. In the second dataset, only the sleep parameters of MSLT were analyzed in the same way as above. All analyzes were judged to be significant when p < 0.05.
RESULTSBaseline Characteristics of NT1 and NT2 PatientsIn the first MSLT, 58 patients were identified as NT1 and 16 as NT2, respectively. Table 1 compared the differences between the demographic characteristics and sleep parameters of the two narcolepsy patients. Body mass index (BMI) of NT1 and NT2 were 25.29 and 23.38 kg/m2, respectively, which was statistically significant (p = 0.035). Moreover, the sleep paralysis rate of NT1 was 60.3%, and that of NT2 was 12.5%, demonstrating a statistically great difference (p = 0.001). In addition, the NT1 group was found to show more hypnagogic hallucination than the NT2 group, which was different to a large extent (p = 0.009).
During MSLT performed for NT1 and NT2 groups, several differences were observed in some parameters. Mean sleep latency (MSL) was 2.00 ± 1.89 and 3.11 ± 2.26 for NT1 min and NT2 groups, respectively, indicating a longer pattern in the NT2 group, which was statistically significant (p = 0.032). As for the average number of SOREMPs, 3.29 ± 1.08 for NT1 and 2.56 ± 1.15 for NT2 were observed, showing more frequent SOREMPs in NT1 group (p = 0.010).
On the other hand, rapid eye movement sleep latency and SOREMP in nocturnal PSG, were not considerably different between NT 1 and NT 2.
Multiple Sleep Latency Test Parameter Change in NT 1 and NT 2 in Follow-Up Multiple Sleep Latency TestWhen MSLT was followed-up in NT 1 group and NT 2 group, the rate of NT 1 patients who showed negative results of MSLT was much lower than NT 2 patients (negative MSLT at follow-up rate of 6.9% and 50.0% in NT1 and NT2, respectively) (Table 2). Particularly, in the case of NT2, among the narcolepsy criteria of ICSD-3, the ratio of not meeting the criteria of more than 2 SOREMPs and MSL ≤ 8 minutes was higher than that of the NT1 group (1.7% in NT 1 and 18.8% in NT 2). Also, in the group that did not meet the MSLT diagnostic criteria at the follow-up MSLT, the proportion of the group who did not satisfy the SOREMP diagnostic criteria of the MSLT parameter was higher than that of the MSL diagnostic criteria. Furthermore, in all the groups with change of MSLT, the groups under negative SOREMP ≥ 2 were observed to be accompanied by negative MSL at follow-up.
Results on the Diagnostic Changes after Follow-Up Multiple Sleep Latency TestIn the case of the NT 1 group, when the second MSLT was conducted, 93.10% (n = 54) was maintained as NT1, 5.17% (n = 3) changed to IH, and 1.72% (n =1) diagnosed as normal (Fig. 1). However, in NT 2 group patients (n = 16), when the 2nd MSLT was carried out, the NT 2 diagnosis was maintained at 50.00% (n = 8), 31.25% changed to IH (n = 5), and 18.75% (n = 3) diagnosed as normal (Fig. 2).
DISCUSSIONThis study is one of the longitudinal studies that analyzed the repeated MSLT results in patients with NT1 and NT 2 in the sleep center of the St. Vincent’s Hospital, College of Medicine, Catholic University of Korea. Notably, distinct differences have been demonstrated among the baseline demographic characteristics and the MSLT. Also, in the case of the repeated MSLT parameter, considerable differences were observed for the two groups.
Firstly, our results of the follow-up MSLT findings in NT 2 groups is in same line with the previous studies [3-7,10-13]. The proportion of maintaining diagnosis in NT2 was only about 50%. Several reasons could be suggested for the sensitivity and specificity of MSLTs. Preferentially, some of the variability resulting from the MSLT may be contributed to methodological problems. Despite the American Academy of Sleep Medicine published clear guidelines for the performance of MSLT, it has been occurred that the specific protocols often differ among sleep labs (i.e., the quantity of the last night’s sleep, timing of the first nap in relation to habitual sleep times and duration, performing 4 vs. 5 naps, optimal nap durations, rigor in ensuring wakefulness among nap opportunities, and methods to score SOREMPs) [14,15]. Furthermore, SOREMP is often expressed as false-positive [13]. In this regard, a previous study reported that subpopulations with excessive sleepiness, including shift workers, young adults with chronic sleep restriction, and patients with sleep apnea, appeared to have a greater prevalence of SOREMP [13,16]. In our study, special efforts were made to exclude the cofounders by asking the participants about the confounding factors (i.e., shift workers, having sleep apnea before, etc.).
Secondly, as initially expected, the NT 1 group and NT 2 group showed some differences in the baseline characteristics. NT 1 group demonstrated a larger value of BMI than NT 2 and more sleep paralysis and hypnogogic hallucination, which was consistent with the previous studies [17]. This difference could be explained by hypocretin/orexin deficiency, which also means NT 1 has nocturnal-sleep wake instability as compared to NT 2 [17,18]. On the other hand, when NT 1 patients repeated MSLT, the proportion of diagnosis retention was greatly high amounting to 93%. It is well known that NT 1 is a well-formed disease, showing a stable course and consistency in nocturnal PSG or MSLT parameters [7,19]. Sleep paralysis was also more common in NT 1 group. One study revealed that several symptoms of narcolepsy disorder were frequently present in families associated with patients who suffered from narcolepsy disorder (i.e., simpleplex families with one narcolepsy patient, and multiplex families with two or more narcolepsy patients in families) [20]. In particular, the incidence and chronicity of hypersomnolence and prevalence of cataplexy-like symptom were observed to be higher in multiplex families than in simple families. Moreover, prevalence of sleep paralysis, incidence and chronicity of hypnagogic hallucination were greater in the multiple family compared to the simple family [20]. This suggests that the above-mentioned narcolepsy symptoms were more genetically influenced [20]. Notably, according to our study, BMI, sleep paralysis, and hypnagogic hallucination were significantly higher in NT 1 than in the parallel NT 2 group, with nocturnal sleep disturbance also greater in NT 1, although not statistically significant. From these results, it could be concluded that the five major symptoms of the narcolepsy, which are cataplexy, sleep paralysis, hypnogogic hallucination, hypersomlenonece, and nocturnal sleep disturbance, came out more clearly in NT 1 as compared to the corresponding NT 2 group.
Thirdly, when analyzing the data of follow-up MSLT in narcolepsy patients, we inferred that the change in SOREMP could have a greater effect on the alteration of diagnosis. In all the groups with the change of MSLT, the groups under negative SOREMPs ≥ 2 were observed to be accompanied by negative MSL at follow-up. It should be noted, however, that there is an evident limitation that the number of participants is relatively small. In addition, several studies have placed more emphasis on SOREMP on PSG as a helpful indicator of high specificity to distinguish between narcolepsy and non-narcoleptic central hypersomnia [21,22]. In their research, Dietmann et al. [21] reported that two or more SOREMPs in either two of the MSLT naps or one SOREMP in PSG and at least one SOREMP in MSLT naps had a high sensitivity of 90% and specificity of 95% with a positive predictive value of 91%, thus successfully differentiating narcoleptic from non-narcoleptic patients. According to our data, it was observed that the baseline nocturnal PSG SOREMP in narcolepsy type 2 was 43.8%, and the maintenance rate of narcolepsy type 2 diagnosis was 50%. Indeed, the rest of 50% of the participants at follow-up was led to an alteration in their diagnosis to non-narcoleptic hypersomnia (IH or normal).
Recently, nocturnal PSG has been spotlighted as an alternative option for diagnosing NT1. In one study, following-up of NT 1 and NT 2 patients, respectively, NT 1 patients showed increase in N1 stage in nocturnal PSG compared to NT 2 patients [17]. Interestingly, some research groups suggested that the sequence of sleep stages on MSLT might be diagnostically helpful, as SOREMPs commonly followed N1 sleep in narcolepsy but not in other disorders [23,24]. It was contended that the rapid transition into REM sleep might reflect the REM sleep dysregulation of narcolepsy [23,24]. In view of the results above, it is likely that the analysis of MSLT, including sleep stages in nocturnal PSG, may help us diagnose narcolepsy in a more accurate manner.
The limitations intrinsic to this study are as follows: To begin with, our sample size was relatively small, with the sample derived from only one single sleep center, thus making it difficult to generalize the results. Besides, the follow-up MSLT was performed just twice, baseline and follow-up, and follow-up intervals were not the same among patients. Therefore, the results obtained through this research could not reflect the detailed course of parameter changes until follow-up. Moreover, because this study is designed as a cohort study, there is a high probability that patients who have been tested twice in this study had a different course of the disease from in many cases. From this fact, the selection bias could not be excluded. Besides, most of the patients undergoing repeated examinations are taking stimulants or anti-depressants because of the abnormal patterns of REM sleep (cataplexy, hallucinations, nightmares, etc.). Even though we educated patients to stop taking the drugs for more than 2 weeks for the test, it is hard for us to exclude the actual number of patients who continued the drug without reporting to the medical staff during the period. As a result, it is difficult to completely rule out of the drug effect. This study did not statistically compare the two groups of people whose diagnosis changed and those who did not. This is because the number of changes in diagnosis was too small to find a statistically significant, so it seems necessary to do it in a follow-up study. However, all NT 2 patients whose diagnosis has changed failed to meet the SOREMP as much as the diagnostic criteria, so SOREMP will need to be observed more carefully when performing MSLT in the future.
In conclusion, the MSLT measures were observed to be a good diagnostic tool for NT 1 patients, but have some limitations when diagnosing patients suffering from NT 2 because of inconsistency. Therefore, it is crucial to repeat the MSLT regularly to confirm the diagnosis in an accurate manner. Other biomarkers, if available, would be helpful for us to distinguish central hypersomnia. Concurrently, understanding the pathophysiology of type 2 narcolepsy appears to be conducive to accurate diagnosis of the patients. To end, a multi-site prospective study should be helpful to diagnose central hypersomnolence, such as objective measures of sleep history (sleep recordings and actigraphs), circadian phase assessments (dim light melatonin onset), and neuropsychological tests.
NOTESAvailability of Data and Material
The datasets generated or analyzed in this study are available from the corresponding author through reasonable request.
Authors’ Contribution
Conceptualization: all authors. Data curation: Hong-Shik Chun, SungMin Kim. Formal analysis: Hong-Shik Chun, Yoo Hyun Um. Investigation: Hong-Shik Chun, Sung-Min Kim. Methadology: Seung-Chul Hong, Tae-Won Kim. Supervision: Ho-Jun Seo, Jong-Hyun Jeong. Writing—original draft: Hong-Shik Chun. Writing—review & editing: Seung-Chunl Hong, Tae-Won Kim.
REFERENCES1. American Academy of Sleep Medicine. International classification of sleep disorders (ICSD-2). 2nd ed. Darien, IL: American Academy of Sleep Medicine 2005.
2. American Academy of Sleep Medicine. International classification of sleep disorders (ICSD-3). 3rd ed. Darien, IL: American Academy of Sleep Medicine 2014.
3. Seong MJ, Choi SJ, Hong SB, Joo EY. Test-retest reliability of multiple sleep latency test in diagnosis of narcolepsy. J Sleep Med 2020;17:175-80.
5. Goldbart A, Peppard P, Finn L, Ruoff CM, Barnet J, Young T, et al. Narcolepsy and predictors of positive MSLTs in the Wisconsin sleep cohort. Sleep 2014;37:1043-51.
6. Trotti LM, Staab BA, Rye DB. Test-retest reliability of the multiple sleep latency test in narcolepsy without cataplexy and idiopathic hypersomnia. J Clin Sleep Med 2013;9:789-95.
7. Huang YS, Guilleminault C, Lin CH, Chen CH, Chin WC, Chen TS. Multiple sleep latency test in narcolepsy type 1 and narcolepsy type 2: a 5-year follow-up study. J Sleep Res 2018;27:e12700.
8. Hong SC, Lin L, Jeong JH, Shin YK, Han JH, Lee JH, et al. A study of the diagnostic utility of HLA typing, CSF hypocretin-1 measurements, and MSLT testing for the diagnosis of narcolepsy in 163 Korean patients with unexplained excessive daytime sleepiness. Sleep 2006;29:1429-38.
9. Um YH, Kim TW, Jeong JH, Seo HJ, Han JH, Kim SM, et al. A longitudinal follow-up study on multiple sleep latency test and body mass index of patients with narcolepsy type 1 in Korea. J Clin Sleep Med 2017;13:1441-4.
10. Lopez R, Doukkali A, Barateau L, Evangelista E, Chenini S, Jaussent I, et al. Test–retest reliability of the multiple sleep latency test in central disorders of hypersomnolence. Sleep 2017;40:zsx164.
11. Ruoff C, Pizza F, Trotti LM, Sonka K, Vandi S, Cheung J, et al. The MSLT is repeatable in narcolepsy type 1 but not narcolepsy type 2: a retrospective patient study. J Clin Sleep Med 2018;14:65-74.
12. Han SJ, Joo EY, Cho JW, Hong SB. The usefulness of repeated multiple sleep latency test for the diagnosis of narcolepsy. J Korean Sleep Res Soc 2008;5:39-42.
13. Baumann CR, Mignot E, Lammers GJ, Overeem S, Arnulf I, Rye D, et al. Challenges in diagnosing narcolepsy without cataplexy: a consensus statement. Sleep 2014;37:1035-42.
14. Dauvilliers Y, Siegel JM, Lopez R, Torontali ZA, Peever JH. Cataplexy--clinical aspects, pathophysiology and management strategy. Nat Rev Neurol 2014;10:386-95.
15. Berry RB, Brooks R, Gamaldo C, Harding SM, Lloyd RM, Quan SF, et al. AASM Scoring Manual Updates for 2017 (Version 2.4). J Clin Sleep Med 2017;13:665-6.
16. Singh M, Drake CL, Roth T. The prevalence of multiple sleep-onset REM periods in a population-based sample. Sleep 2006;29:890-5.
17. Um YH, Oh J, Kim SM, Kim TW, Seo HJ, Jeong JH, et al. Differential characteristics of repeated polysomnography and multiple sleep latency test parameters in narcolepsy type 1 and type 2 patients: a longitudinal retrospective study. Sleep Breath 2022;26:1939-46.
18. Maski KP, Colclasure A, Little E, Steinhart E, Scammell TE, Navidi W, et al. Stability of nocturnal wake and sleep stages defines central nervous system disorders of hypersomnolence. Sleep 2021;44:zsab021.
19. Almeneessier AS, Alballa NS, Alsalman BH, Aleissi S, Olaish AH, BaHammam AS. A 10-year longitudinal observational study of cataplexy in a cohort of narcolepsy type 1 patients. Nat Sci Sleep 2019;11:231-9.
20. Ohayon MM, Black J, Krystal AD, Shapiro CM, Swick TJ, Bogan R, et al. Longitudinal study of narcolepsy symptoms in first, second, and third-degree relatives of simplex and multiplex narcolepsy families. Sleep Med 2019;53:88-93.
21. Dietmann A, Gallino C, Wenz E, Mathis J, Bassetti CLA. Multiple sleep latency test and polysomnography in patients with central disorders of hypersomnolence. Sleep Med 2021;79:6-10.
22. Andlauer O, Moore H, Jouhier L, Drake C, Peppard PE, Han F, et al. Nocturnal rapid eye movement sleep latency for identifying patients with narcolepsy/hypocretin deficiency. JAMA Neurol 2013;70:891-902.
Fig. 1.Repeatability of MSLT among NT1 patients (n = 58). MSLT, multiple sleep latency test; NT1, narcolepsy type 1; IH, idiopathic hypersomnia. 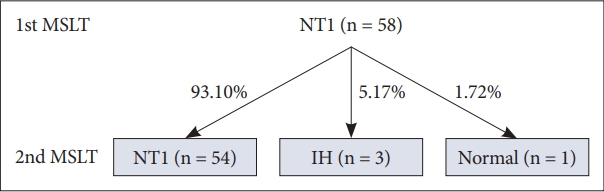
Fig. 2.Repeatability of MSLT among NT2 patients (n = 16). MSLT, multiple sleep latency test; NT2, narcolepsy type 2; IH, idiopathic hypersomnia. 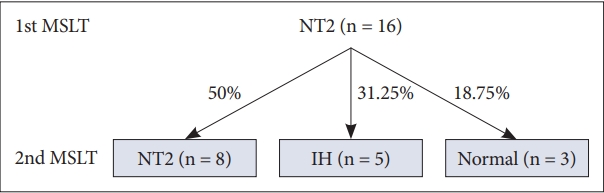
Table 1.Demographic, clinical, and laboratorial findings of narcolepsy patients
Table 2.Results of follow-up MSLT in patients diagnosed as narcolepsy
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||