AbstractBackground and ObjectiveWe considered the concept of the DBST, the discrepancy between a patient’s desired time in bed (TIB) and desired total sleep time (TST). The DBST index can be used to easily assess a patient’s thoughts on their desired TST and dysfunctionally long TIB. This study aimed to explore whether the DBST index can predict the severity of insomnia.
MethodsA total of 374 members of the general population participated in this e-survey study. The participants answered questions regarding their bedtime, sleep onset time, wake-up time, desired TST, and desired TIB, and psychological symptoms were assessed using the Insomnia Severity Index (ISI), Patients Health Questionnaire–9 items (PHQ-9), Dysfunctional Beliefs and Attitudes about Sleep–16 items (DBAS-16), and Glasgow Sleep Effort Scale (GSES).
ResultsThe DBST index was significantly correlated with the ISI (r = 0.20, p < 0.01), PHQ-9 (r = 0.15, p < 0.01), GSES (r = 0.14, p < 0.01), DBAS-16 (r = 0.16, p < 0.01), desired TST (r = -0.62, p < 0.01), and desired TIB (r = 0.52, p < 0.01). Linear regression analysis showed that insomnia severity was predicted by persistent preoccupation with sleep (beta = 0.64, p < 0.001), dysfunctional beliefs about sleep (beta = 0.06, p < 0.001), depression (beta = 0.23, p < 0.001), and DBST (beta = 0.32, p = 0.035). The DBST directly influenced insomnia severity, and this association was shown to be mediated by dysfunctional beliefs and attitudes about sleep, preoccupation with sleep, and depression.
INTRODUCTIONInsomnia is a common disturbing complaint that can influence patients’ psychological states, mood states, or quality of life [1]. In general, 7–8 h of sleep is recommended for adults. Numerous studies have shown a U-shaped relationship between self-reported sleep length and physical health such as hypertension [2], obesity [3], metabolic syndrome [4], stroke [5], cardiovascular risk [6], and all-cause mortality [7-9], and even mental health factors, including depression [10] and cognitive impairment [11]. Although the harmful effect of long sleep duration is controversial [12], the harmful effect of short sleep duration is well known. Based on these results, it is speculated that around 7–8 h of sleep can promote better health outcomes.
However, in the concept of dysfunctional beliefs about sleep, this “sufficient total sleep time (TST)” of 7–8 h sometimes may exert a psychological burden on some individuals. The perception that one should sleep at least 7–8 h a day to maintain their health status may often induce negative emotions, such as fear or anxiety, that prevent them from sleeping well [13]. Therefore, it is important to evaluate a patient’s dysfunctional beliefs on their sufficient sleep duration when Cognitive-Behavior Therapy for Insomnia (CBT-I) [14] is applied to insomnia patients.
Desired Total Sleep Time and Desired Time in BedIn clinical practice, it is commonly observed that patients who experience insomnia often want to go to bed early in the evening to achieve an early sleep onset. They often believe that early bedtime may induce the early onset of sleep [14,15], and some individuals believe that going to bed early is a healthy behavior [16]. Based on these beliefs, patients with insomnia tend to go to bed early in the evening after taking sleeping pills [17]. However, an early bedtime can lead to tension or anxiety that further impairs the ability to sleep [18,19], and taking sleeping pills early in the evening is reported to be associated with decreased satisfaction with pills [17]. Another problem with an early bedtime is that it might lead to a long time in bed (TIB). If one goes to bed early in the evening and wakes up early in the morning, sleep problems like a state of advanced type of circadian rhythm sleepwake disorder would be likely to occur. If one can accept their advanced sleep phase, it might work as a sleep strategy. However, if one wants to sleep until approximately 6 or 7 am, early bedtime inevitably causes a long TIB. A long TIB may result in low sleep efficiency (SE; calculated as TST/TIB, %), resulting in poor sleep quality [20].
Sleep regulation can be explained by the two-process model [21,22], one of the most prevalent conceptual models of sleep regulation, which states that sleep regulation involves the interaction of a homeostatic process (Process S) and a circadian pacemaker (Process C). Process S reflects that sleep can be forced by prolonged wakefulness [21,22]. We have previously reported that patients with short sleep latency (≤ 30 min) tend to go to bed late in the evening [23]. In the same study, we estimated the duration from wake-up time to bedtime (WTB) among patients with insomnia and reported that 16.5 ± 1.1 h of WTB in patients with short sleep latency compared to 15.8 ± 1.5 h of WTB in patients with long sleep latency (> 30 min). Furthermore, a long WTB was significantly correlated with short sleep latency. This indicates that sleep pressure (homeostatic drive) stemming from a long period of wakefulness is required to promote good sleep, and forcing an early bedtime does not effectively induce sleep since it might decrease periods of wakefulness.
We further reported the association between sleeping pill administration time and patients’ subjective satisfaction with their sleeping pills [17]. We observed that patients who were satisfied with their sleeping pills tended to take them later than patients who were not satisfied with their sleeping pills. In parallel with the WTB, late administration of sleeping pills results in a shorter duration from pill administration to wake-up time (PTW) and might increase the WTB of patients.
Concept of the DBST Index; the Discrepancy between Desired Time in Bed and Desired Total Sleep TimeBased on the mean sleep duration of adults, 7–8 h of sleep per night is recommended. However, some patients with insomnia who cannot easily fall asleep or maintain their sleep well, say, “My only wish is to have at least 5–6 h of sleep!” Although this may only be an individual stating that they desperately want to sleep well, it reveals some of the dysfunctional beliefs about sleep. If one wants at least 6 h of sleep and wants to fall asleep early in the evening, they should wake up early in the morning; to achieve 6 h of TST from a 9-pm bedtime, the wake-up time should be at 3 am. However, the common wake-up time is approximately 6–7 am. When a clinician asks them, “From what time to what time do you want to sleep?” they may answer that they want to sleep longer than they desire; for example, from 10 pm to 7 am (around 9 h of TIB). This ‘dysfunctionally’ long TIB may decrease SE. Based on the concept of the sleep restriction technique in CBT-I, shortening the TIB is effective for improving SE. Therefore, there is a need to assess the ‘dysfunctionally’ long TIB among patients with insomnia to improve their sleep.
We considered the concept of the discrepancy between a patient’s desired TIB and desired TST, the DBST, which can easily assess patients’ thoughts on their desired TST and dysfunctionally long TIB. If patients suffer from severe insomnia, they may desperately want to sleep at least a few hours, but at the same time, they may want an early bedtime and late wake-up time. As the discrepancy is high, we can speculate that patients may suffer severe insomnia or a high level of dysfunctional beliefs about sleep. A recent study reported that the severity of insomnia was influenced by depression, sleep preoccupation, dysfunctional sleep beliefs, and DBST index in the general population [24]. The first objective in this replication study is to investigate the usefulness of DBST index again, since this concept isn’t still valid. Second, the previous study did not use a rating scale that could assess dysfunctional beliefs about sleep like the Dysfunctional Beliefs and Attitudes about Sleep (DBAS). Third, this study explores the correlation between the DBST and subjective sleep indices such as bedtime, sleep onset time, wake-up time, sleep onset latency, or TIB, since these were not evaluated in the previous research. Though it was hypothesized that the DBST could predict the severity of insomnia among patients with insomnia, the DBST concept was applied to the general population in the current study prior to applying the concept to patients with clinical insomnia. This study aimed to explore whether the DBST can predict the severity of insomnia among the general population. Furthermore, we explored whether dysfunctional beliefs about sleep, preoccupation with sleep, or depression may mediate the influence of DBST index on insomnia severity. We hypothesized that 1) the DBST index will be positively related to insomnia severity, 2) dysfunctional beliefs about sleep will be positively associated with insomnia severity, 3) persistent preoccupation with sleep will be positively associated with insomnia severity, 4) depression will be positively associated with insomnia severity, 5) dysfunctional beliefs about sleep will partially mediate the relationship between the DBST index and insomnia severity, 6) persistent preoccupation with sleep partially mediate the relationship between the DBST index and insomnia severity, and 7) depression will partially mediate the relationship between the DBST index and insomnia severity.
METHODSParticipants and ProcedureThis study was conducted using an online survey administered to members of the general public in Korea. This anonymous online survey was conducted by a professional survey company (EMBRAIN, Seoul, Korea) from January 10 to January 18, 2022. Of the 14 million panelists of the survey company, 400 voluntarily participated in this study, and information on the participants’ age, sex, living region, marital status, past psychiatric history, and current psychiatric distress were collected. Participants who answered that they were shift workers whose sleep pattern was irregular [25,26] were not included. We developed the survey form according to the Checklist for Reporting Results of Internet e-Surveys guidelines [27]. The study protocol was approved by the Institutional Review Board (IRB) of the Asan Medical Center (2021-1755), and the requirement for written informed consent was waived by the IRB.
The sample size of 400 was estimated based on the allocation of 40 samples for 10 cells; biological sex (males and females) × five age groups (18–29, 30–39, 40–49, 50–59, 60–80) [28]. And also, sample size required to determine whether a correlation coefficient differs from zero were 396 (type I error (α) = 0.05, type II error (β) = 0.15, and expected correlation coefficient = 0.15). The survey company randomly sent 3000 emails for enrollment to their registered panelists, and 949 participants accessed the survey, and 468 completed the survey. After eliminating responses with too short or long response speed [29], all 400 responses were finally collected (response rate = 13.3%, 400 of 3000).
MeasuresSleep indicesIn this study, sleep indices were defined as time variables (bedtime, sleep onset time, and wake-up time), duration variables (sleep onset latency and TIB), and DBST. Sleep indices were calculated based on participants’ responses to the questions included in the survey: “What is your usual bedtime?” “What is your usual time to fall asleep?” and “What is your usual time to finally get out of bed in the morning?” Time variables such as bedtime, sleep onset time, and wake-up time were obtained by averaging the usual times reported. If a participant answered that they usually went to bed between 9:00 and 10:00 pm, we estimated the bedtime as 9:30 pm. These time variables were transformed into numeric variables using 60 min as 1 unit and 30 min (half of 1 h) as 0.50 units (i.e., 9:30 pm was transformed into 21.5) [17]. Duration variables, including sleep onset latency and TIB, were estimated using the time variables.
In this study, we also proposed a new sleep index, the DBST, defined as the difference between one’s desired TIB and one’s desired TST. The desired TST was assessed with the question: “How many hours do you want to sleep per day?” and the desired TST was estimated by averaging the responded hours; for example, if a participant answered that they wanted to sleep for 7–8 h, we estimated the desired TST as 7.5 h. The desired TIB was assessed using the question “From what time to what time do you want to sleep?” and the desired TIB was estimated by the duration of the response. If a participant answered that they wanted to sleep from 11:30 pm to 7:00 am, we estimated the desired TIB as 7.5 h. Finally, the DBST was calculated as [desired TIB] - [desired TST].
Insomnia Severity IndexThe Insomnia Severity Index (ISI) is a self-rating scale developed to assess one’s severity of insomnia [30], consisting of seven items rated on a 5-point Likert-like scale. A higher total score indicates more severe insomnia. In this study, we applied the Korean version of the ISI [31], and Cronbach’s alpha for our sample was 0.801.
Patient Health Questionnaire–9 itemsThe Patient Health Questionnaire–9 items (PHQ-9) is a self-reported rating scale used to measure one’s severity of depression [32], consisting of nine items rated on a 4-point Likert-like scale ranging from 0 (not at all) to 3 (nearly every day). A higher total PHQ-9 score, ranging from 0 to 27, reflects a severe level of depression. In this study, we applied the Korean version of the PHQ-9 [33], and Cronbach’s alpha for our sample was 0.886.
Glasgow Sleep Effort ScaleThe Glasgow Sleep Effort Scale (GSES), a self-report rating scale to assess one’s persistent preoccupation with sleep [34], consists of seven items rated on a 3-point Likert-like scale ranging from 0 (not at all) to 2 (very much). A higher total score, ranging from 0 to 14, reflects a greater preoccupation with sleep. In this study, we applied the Korean version of GSES [35], and Cronbach’s alpha for these samples was 0.754.
Dysfunctional Beliefs and Attitudes about Sleep–16 itemsThe DBAS-16, a self-reported rating scale to measure one’s dysfunctional beliefs about sleep [36], consists of 16 items rated on 100-mm visual analog scales. The final averaged total score was calculated by adding the scores for all 16 items and dividing by 16. In this study, we applied the Korean version of the DBAS-16 scale [37], and Cronbach’s alpha for our sample was 0.898.
Statistical AnalysisData are summarized as mean ± standard deviation, and the significance level was defined as p < 0.05 on two-tailed tests for all analyses. Pearson’s correlation coefficients were determined to examine the association between DBST and participants’ clinical variables, including sleep indices and psychological symptom ratings. Linear regression analyses were used to explore the variables that may predict the severity of each participant’s insomnia severity. Causal mediation analysis was conducted utilizing the R package ‘mediation (version 4.5.0; R Foundation for Statistical Computing, Vienna, Austria)’ [38] for estimating the average causal mediation effect (ACME), average direct effect (ADE), and percentage of total mediation effect. On the other hand, the Generalized Linear Models mediation analysis was performed by implementing the bootstrap method with 2000 resamples to examine the mediating effect of the psychological symptoms on the association between DBST and insomnia severity. SPSS version 21.0 (IBM Co., Armonk, NY, USA), AMOS version 27 (IBM Co.), Jamovi version 1.6.23 (https://www.jamovi.org), and R studio were used for statistical analyses.
RESULTSAmong the 400 participants, 374 were analyzed after excluding 26 participants who did not completely respond to all questions. The participants were residents of Seoul (n = 122, 32.6%), Pusan (n = 21, 5.6%), Daegu (n = 3, 0.8%), Incheon (n = 22, 5.9%), Gwangju (n = 6, 1.6%), Daejeon (n = 9, 2.4%), Ulsan (n = 7, 1.9%), Gyeonggi Province (n = 129, 34.5%), Gangwon Province (n = 4, 1.1%), Chungcheong Province (n = 18, 4.8%), Jeolla Province (n = 11, 2.9%), Gyeongsang Province (n = 8, 2.2%), Jeju Province (n = 9, 2.4%), and Sejong (n = 5, 1.3%). Table 1 shows the clinical characteristics of the participants.
Table 2 shows the results of correlation analysis. The ISI score was significantly correlated with PHQ-9 (r = 0.48, p < 0.01), GSES (r = 0.57, p < 0.01), DBAS-16 (r = 0.53, p < 0.01), sleep onset time (r = 0.15, p < 0.01), sleep onset latency (r = 0.24, p < 0.01), desired TIB (r = 0.15, p < 0.01), and the DBST index (r = 0.20, p < 0.01). The DBST index was significantly correlated with ISI (r = 0.20, p < 0.01) (Fig. 1), PHQ-9 (r = 0.15, p < 0.01), GSES (r = 0.14, p < 0.05), DBAS-16 (r = 0.16, p < 0.01), desired TST (r = -0.62, p < 0.01), and desired TIB (r = 0.52, p < 0.01).
Linear regression analysis, performed with the enter method, showed that persistent preoccupation with sleep (GSES, beta = 0.64, p < 0.001), dysfunctional beliefs about sleep (DBAS-16, beta = 0.06, p < 0.001), depression (PHQ-9, beta = 0.23, p < 0.001), and the DBST index (beta = 0.32, p = 0.035) could be used to predict insomnia severity (adjusted R2 = 0.44, F = 49.6, p < 0.001) (Table 3).
Table 4 and Fig. 2 show the results of causal mediation analysis. The mediation hypotheses were confirmed, since results revealed significant relative indirect effects of dysfunctional belief about sleep (ACME = 0.32; 95% confidence interval [CI], 0.11 to 0.57) on the association between the DBST index and insomnia severity. And also, persistent preoccupation with sleep (ACME = 0.29; 95% CI, 0.07 to 0.50) and depression (ACME = 0.27; 95% CI, 0.07 to 0.49) have mediation effect on the association between the DBST index and insomnia severity. Among these components, dysfunctional beliefs about sleep have a highest mediation effect with a proportion of mediation (41%). Generalized Linear Modeling mediation analysis also revealed that the DBST directly influenced insomnia severity, and this association was shown to be mediated by depression, dysfunctional beliefs and attitudes about sleep, and preoccupation with sleep (Table 5 and Fig. 3).
DISCUSSIONIn this pilot study, the DBST index was tested as a new sleep index for quantifying the difference between desired TIB and desired TST. In addition, we applied the DBST index concept for assessing insomnia severity among the general population using subjective rating scales prior to applying the DBST concept to a clinical sample of patients with insomnia using objective measures, like nocturnal polysomnography. Insomnia severity could be predicted by the DBST index, depression, preoccupation with sleep, and dysfunctional beliefs about sleep. In the mediation analysis, the DBST index directly influenced the insomnia severity of the general population, and this association was mediated by depression, preoccupation with sleep, and dysfunctional beliefs about sleep.
DBST and Insomnia SeverityThis pilot study explored whether the DBST is a feasible concept to predict insomnia severity among the general population. The DBST index was significantly correlated with insomnia severity and depression, preoccupation with sleep, and dysfunctional beliefs about sleep. In clinical practice, the DBST can be useful to assess and manage patients’ insomnia symptoms. Individuals often do not realize the time when they should go to bed, fall asleep, or wake up. It is a concept similar to the sleep restriction technique of the CBT-I. In a previous study, we reported that 17 h of wakefulness is required for short sleep latency [23], and administering sleeping pills 7 h before the waking-up time increases satisfaction with sleeping pills [17]. The results showed that around 17 h of wakefulness is needed for good sleep. This agrees with process S of the two-process model [21,22]. Therefore, the concept of DBST shows that clinicians should consider the wake-up time in the morning when recommending the time at which patients should go to bed. To decrease the DBST, clinicians should consider the desired TST when recommending the time to go to bed in the evening and the time to wake up in the morning. Of course, clinicians should also simultaneously consider that patients’ desired TST might be intentionally shortened, as they may “only wish to have at least 6 h of sleep.”
In this study, the DBST index was one of the variables that may predict insomnia severity in the general population. Based on the results, patients whose DBST is high may experience severe insomnia, and greater DBST may be correlated with low SE since a long TIB may contribute to low SE. Since it has been reported that low SE was correlated with high levels of insomnia severity [8,39], the DBST index also may be correlated with insomnia severity. Previously, we reported that a longer duration from WTB predicts a short sleep latency [23]. Since greater DBST may decrease the duration from wake-up to bedtime, it may also induce a longer sleep onset latency. Nevertheless, we should address some limitations of the DBST concept in a future study. First, the DBST index concept did not include desired napping times which can also reduce homeostatic drive. Second, we need to explore what the negative DBST value means. Although most likely positive in the context of insomnia, the negative DBST might reflect insufficient sleep time and contribute to short sleep duration. Third, the association of the DBST index with objective measures of sleep derived from polysomnography test needs to be explored.
The DBST concept should also be applied when clinicians prescribe sleeping pills. In our previous study, we reported that a shorter interval from sleeping PTW increased subjective satisfaction with sleeping pills [17]. In addition, the duration from the administration of sleeping pills to sleep onset time, rather than to bedtime, predicted patients’ satisfaction with sleeping pills [17]. Based on these data, decreasing the duration from sleeping pill administration to sleep onset time by delaying the sleeping pill administration time may be effective for increasing patients’ satisfaction with sleeping pills. Therefore, it was hypothesized that the administration of sleeping pills and decreasing DBST might be effective in increasing patients’ satisfaction with sleeping pills. Further studies are needed to test this hypothesis.
Mediation Effect of Dysfunctional Beliefs about Sleep, Persistent Preoccupation with Sleep, and Depression on the Association between DBST and Insomnia SeverityWe further observed that DBST directly influenced insomnia severity and dysfunctional beliefs about sleep, persistent preoccupation with sleep and depression partially mediated this association. Dysfunctional beliefs about sleep and a major source of worry and preoccupation with sleep also mediate the association between the DBST and insomnia severity in this study. These erroneous beliefs, which can be counterproductive maladaptive coping strategies, can promote excessive TIB and time spent staying in bed while awake [40]. Patients with high levels of dysfunctional beliefs about sleep are usually anxious about not sleeping well and become preoccupied with sleep problems. Consequently, they tend to go to bed early in the evening to fall asleep early; however, they do not easily fall asleep despite their erroneous beliefs. This may mediate the influence of DBST on insomnia severity. However, this is the first study to explore the association between the DBST and dysfunctional beliefs about sleep or persistent preoccupation with sleep using DBAS-16 or GSES. Further studies need to be conducted among patients with insomnia who can have high levels of dysfunctional beliefs about sleep compared to the general population.
In this study, we also observed depression mediates the influence of the DBST index on insomnia severity. It is well known that depressed mood is related to a delayed sleep phase [41], although circadian rhythms other than sleep-wake are also associated with depression [42]. It has been reported that depressed patients tend to stay in bed longer, go to bed earlier, and wake up later in the morning. This may stem from their depressed mood, feeling of lack of energy, or fatigue symptoms, and treatment of these sleep problems should be a focus when managing depression [43]. These sleep patterns observed among depressed patients might be one of the factors for greater DBST. Another possible explanation is that depression might influence dysfunctional beliefs about sleep and consequently influence the DBST index [44], although we could not confirm it from this study. Further investigation is needed to explore the association between depression and DBST.
This study has several limitations. First, the concept of the DBST is not yet clearly defined: a repetitive examination of whether the DBST concept can be applied in clinical practice should be performed in the future. Additionally, the DBST index concept did not include desired napping times. Daytime naps can also reduce homeostatic drive, and this needs to be clarified in future studies. Second, this study was performed on the general population, not among patients with insomnia. The current study was planned as a pilot study so that the same principles can be applied to patients with clinical insomnia: this latter clinical study is currently being planned. Third, this study was conducted using an anonymous online survey, not face-to-face interviews. Due to constraints associated with the coronavirus disease (COVID-19) pandemic, we conducted the survey online to prevent the risk of COVID-19 transmission. The participants were selected from panelists registered with a survey company, and the selection may therefore be biased. Fourth, sleep indices with standardized subjective tools such as the Pittsburgh Sleep Quality Index [45] or objective measures such as nocturnal polysomnography were not used in this study. A further ongoing study will evaluate the association between the DBST index and standardized subjective or objective measures. Finally, the small sample size of this study may have decreased the statistical power.
In conclusion, insomnia severity could be predicted by the DBST index, depression, preoccupation with sleep, and dysfunctional beliefs about sleep. In the mediation analysis, the DBST index directly influenced the insomnia severity of the general population, and this association was mediated by dysfunctional beliefs about sleep, persistent preoccupation with sleep, or depression. The DBST concept can be applied as a possible new sleep index to assess and evaluate insomnia severity. Although the DBST is not yet a sound concept, further studies which are underway to explore the DBST index in a clinical sample of patients with insomnia will help develop this novel concept.
NOTESAvailability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
ACKNOWLEDGEMENTSI would like to express my appreciation to all my team members and alumni of the AMC sleep and psycho-oncology lab who aided me in developing the numerous concepts for diagnosis and management of insomnia, such as the DBST, sleeping pill administration time, or TIB over 24 h. Specially, I would like to express my appreciation to Oli Ahmed (Department of Psychology, University of Chittagong, Chattogram, Bangladesh, and National Centre for Epidemiology and Population Health, Australian National University, Canberra, ACT, Australia) for his contribution to conduct the causal mediation analysis.
REFERENCES1. Morin CM. Insomnia: psychological assessment and management. New York: Guildford Press 1993.
2. Fang J, Wheaton AG, Keenan NL, Greenlund KJ, Perry GS, Croft JB. Association of sleep duration and hypertension among US adults varies by age and sex. Am J Hypertens 2012;25:335-41.
3. Brady EM, Bodicoat DH, Hall AP, Khunti K, Yates T, Edwardson C, et al. Sleep duration, obesity and insulin resistance in a multi-ethnic UK population at high risk of diabetes. Diabetes Res Clin Pract 2018;139:195-202.
4. Xie J, Li Y, Zhang Y, Vgontzas AN, Basta M, Chen B, et al. Sleep duration and metabolic syndrome: an updated systematic review and metaanalysis. Sleep Med Rev 2021;59:101451.
5. Li W, Wang D, Cao S, Yin X, Gong Y, Gan Y, et al. Sleep duration and risk of stroke events and stroke mortality: a systematic review and meta-analysis of prospective cohort studies. Int J Cardiol 2016;223:870-6.
6. Gupta K, Nagalli S, Kalra R, Gupta R, Mahmood S, Jain V, et al. Sleep duration, baseline cardiovascular risk, inflammation and incident cardiovascular mortality in ambulatory U.S. adults: national health and nutrition examination survey. Am J Prev Cardiol 2021;8:100246.
7. Shen X, Wu Y, Zhang D. Nighttime sleep duration, 24-hour sleep duration and risk of all-cause mortality among adults: a meta-analysis of prospective cohort studies. Sci Rep 2016;6:21480.
8. Yin J, Jin X, Shan Z, Li S, Huang H, Li P, et al. Relationship of sleep duration with all‐cause mortality and cardiovascular events: a systematic review and dose‐response meta‐analysis of prospective cohort studies. J Am Heart Assoc 2017;6:e005947.
9. Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry 2002;59:131-6.
10. Dong L, Xie Y, Zou X. Association between sleep duration and depression in US adults: a cross-sectional study. J Affect Disord 2022;296:183-8.
11. Liang Y, Qu LB, Liu H. Non-linear associations between sleep duration and the risks of mild cognitive impairment/dementia and cognitive decline: a dose-response meta-analysis of observational studies. Aging Clin Exp Res 2019;31:309-20.
12. Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev 2008;12:289-98.
13. Akram U, Gardani M, Riemann D, Akram A, Allen SF, Lazuras L, et al. Dysfunctional sleep-related cognition and anxiety mediate the relationship between multidimensional perfectionism and insomnia symptoms. Cogn Process 2020;21:141-8.
14. Morin CM. Cognitive-behavioral approaches to the treatment of insomnia. J Clin Psychiatry 2004;65 Suppl 16:33-40.
15. Espie CA. Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol 2002;53:215-43.
16. Liu X, Liu L. Sleep habits and insomnia in a sample of elderly persons in China. Sleep 2005;28:1579-87.
17. Chung S, Youn S, Yi K, Park B, Lee S. Sleeping pill administration time and patient subjective satisfaction. J Clin Sleep Med 2016;12:57-62.
18. Ellis J, Hampson SE, Cropley M. The role of dysfunctional beliefs and attitudes in late-life insomnia. J Psychosom Res 2007;62:81-4.
19. Narisawa H. Anxiety and its related factors at bedtime are associated with difficulty in falling asleep. Tohoku J Exp Med 2013;231:37-43.
20. Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res 2002;53:737-40.
22. Borbély AA, Daan S, Wirz-Justice A, Deboer T. The two-process model of sleep regulation: a reappraisal. J Sleep Res 2016;25:131-43.
23. Chung S, Youn S, Kim C. Are you asking what time did your patients go to bed?: getting the short sleep onset latency. Sleep Med Res 2018;9:58-62.
24. Lee J, Cho IK, Kim K, Kim C, Park CHK, Yi K, et al. Discrepancy between desired time in bed and desired total sleep time, insomnia, depression, and dysfunctional beliefs about sleep among the general population. Psychiatry Investig 2022;19:281-8.
25. Kim HW, Jung SM, Choi YS, Kim SA, Joung HY, Kim EJ, et al. Sleep patterns of firefighters with shift working schedules in Seoul Metropolitan area. Sleep Med Res 2017;8:68-75.
26. Lee S, Bonnar D, Kim Y, Lee Y, Lee S, Gradisar M, et al. Sleep characteristics and risk factors of Korean esports athletes: an exploratory study. Sleep Med Res 2020;11:77-87.
27. Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet e-surveys (CHERRIES). J Med Internet Res 2004;6:e34.
28. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: Lawrence Erlbaum Associates 1988.
29. Conrad FG, Couper MP, Tourangeau R, Zhang C. Reducing speeding in web surveys by providing immediate feedback. Surv Res Methods 2017;11:45-61.
30. Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011;34:601-8.
31. Cho YW, Song ML, Morin CM. Validation of a Korean version of the insomnia severity index. J Clin Neurol 2014;10:210-5.
32. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001;16:606-13.
33. Morin CM, Vallières A, Guay B, Ivers H, Savard J, Mérette C, et al. Cognitive behavioral therapy, singly and combined with medication, for persistent insomnia: a randomized controlled trial. JAMA 2009;301:2005-15.
34. Broomfield NM, Espie CA. Towards a valid, reliable measure of sleep effort. J Sleep Res 2005;14:401-7.
35. Kim MK, Koo HJ, Kwon JH, Han JK. Validation of Korean version of Glasgow Sleep Effort Scale (GSES). Cognitive Behavior Therapy in Korea 2014;14:319-37.
36. Morin CM, Stone J, Trinkle D, Mercer J, Remsberg S. Dysfunctional beliefs aand attitudes about sleep among older adults with and without insomnia complaints. Psychol Aging 1993;8:463-7.
37. Yu ES, Ko YG, Sung GH, Kwon JH. Validation of the Korean version of dysfunctional beliefs and attitudes about sleep (K-DBAS-16). Kor J Clin Psychol 2009;28:309-20.
38. Gunlu A. Development of social distancing phobia scale and its association with anxiety and perceived stress. Int J Ment Health Addict 2021 Oct 7;[Epub]. https://doi.org/10.1007/s11469-021-00664-2.
39. Castronovo V, Galbiati A, Marelli S, Brombin C, Cugnata F, Giarolli L, et al. Validation study of the Italian version of the insomnia severity index (ISI). Neurol Sci 2016;37:1517-24.
40. Perlis ML, Giles DE, Mendelson WB, Bootzin RR, Wyatt JK. Psychophysiological insomnia: the behavioural model and a neurocognitive perspective. J Sleep Res 1997;6:179-88.
41. Richardson C, Gradisar M. Depressed mood and repetitive negative thinking in delayed sleep-wake phase disorder: treatment effects and a comparison with good sleepers. J Sleep Res 2022;31:e13452.
42. Mendlewicz J. Disruption of the circadian timing systems: molecular mechanisms in mood disorders. CNS Drugs 2009;23 Suppl 2:15-26.
Fig. 1.Correlation between insomnia severity and DBST. DBST, discrepancy between desired time in bed and desired total sleep time. 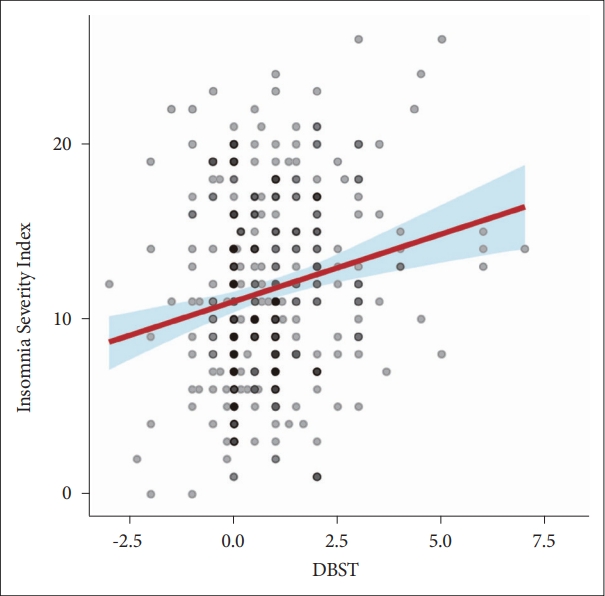
Fig. 2.Mediation effects of dysfunctional beliefs about sleep, persistent preoccupation with sleep, and depression on the influence of the DBST index on insomnia severity. A: Mediator: dysfunctional belief about sleep. B: Mediator: preoccupation with sleep. C: Mediator: depression. ACME, average causal mediation effect; ADE, average direct effect; DBST, discrepancy between desired time in bed and desired total sleep time. 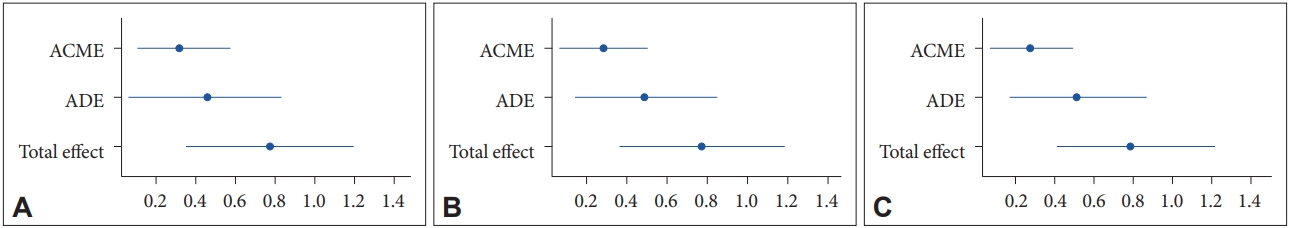
Fig. 3.Generalized Linear Models Mediation model showing the pathway from the discrepancy between the desired time in bed and the desired total sleep time (independent variables) on insomnia severity (outcome) through depression, preoccupation with sleep, or dysfunctional beliefs about sleep (mediator). **p < 0.01. DBST, discrepancy between desired time in bed and desired total sleep time. 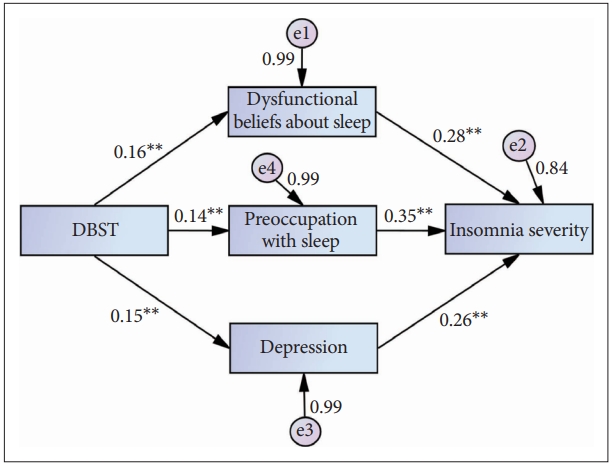
Table 1.Clinical characteristics of the study subjects (n = 374) Values are presented as n (%), mean ± SD, or mean ± SD (range). ISI, Insomnia Severity Index; PHQ-9, Patient Health Questionnaire– 9 items; GSES, Glasgow Sleep Effort Scale; DBS-16, Dysfunctional Beliefs and Attitudes about Sleep–16 items; DBST, discrepancy between desired time in bed and desired total sleep time; SD, standard deviation. Table 2.Pearson’s correlation coefficients of each variable for all participants (n = 374)
Table 3.Linear regression analysis of insomnia severity among the general population Table 4.Results of the causal mediation analysis: mediating role on the influence of the DBST index on the insomnia severity DBST, discrepancy between desired time in bed and desired total sleep time; ACME, average causal mediation effect (indirect effect); ADE, average direct effect; Prop. mediated, the mediator variable explains the percentage of the association between the DBST index and insomnia severity; CI, confidence interval. Table 5.Results of the Generalized Linear Models mediation analysis |
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||