Determining the level of ventilatory support for patients with hypoventilation syndrome with noninvasive positive pressure ventilation (NPPV), attended titration with polysomnography (PSG) is recommended at a consensus level [1]. For patients with chronic alveolar hypoventilation due to restrictive thoracic cage disorders such as kyphoscoliosis, NPPV using bilevel positive airway pressure (PAP) is generally preferred [1]. In many cases, the level of pressure support is determined in the hospital-based on tidal volume, pulse oximetry, and arterial blood gas level largely during the daytime, or set empirically at home guided by the patient’s tolerance [2]. In most literature on NPPV, attended NPPV titration PSG has not been used to select the level of support. Attended NPPV titration PSG is still not widely adopted and used in only selected patients with comorbid obstructive sleep apnea or obesity hypoventilation.
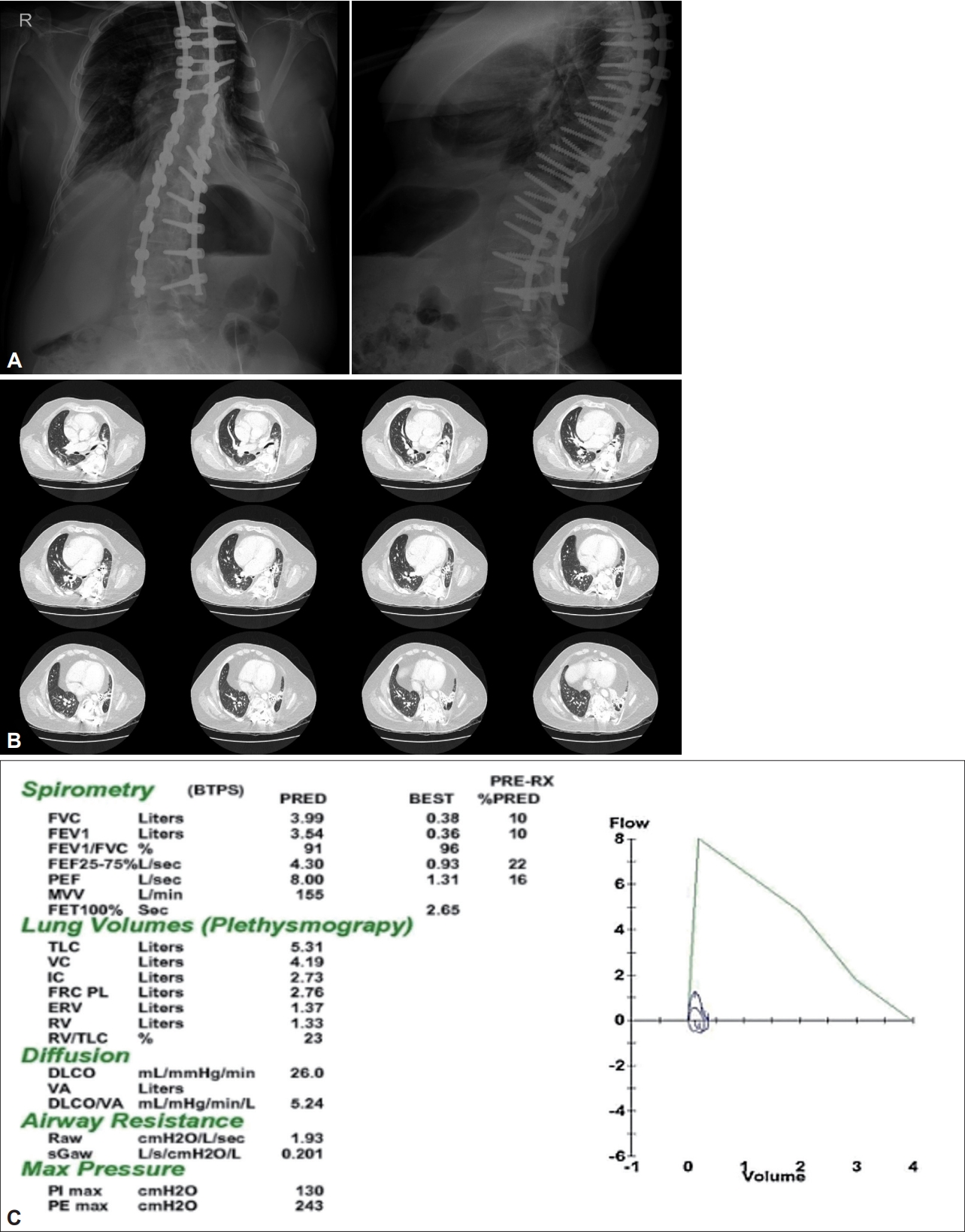
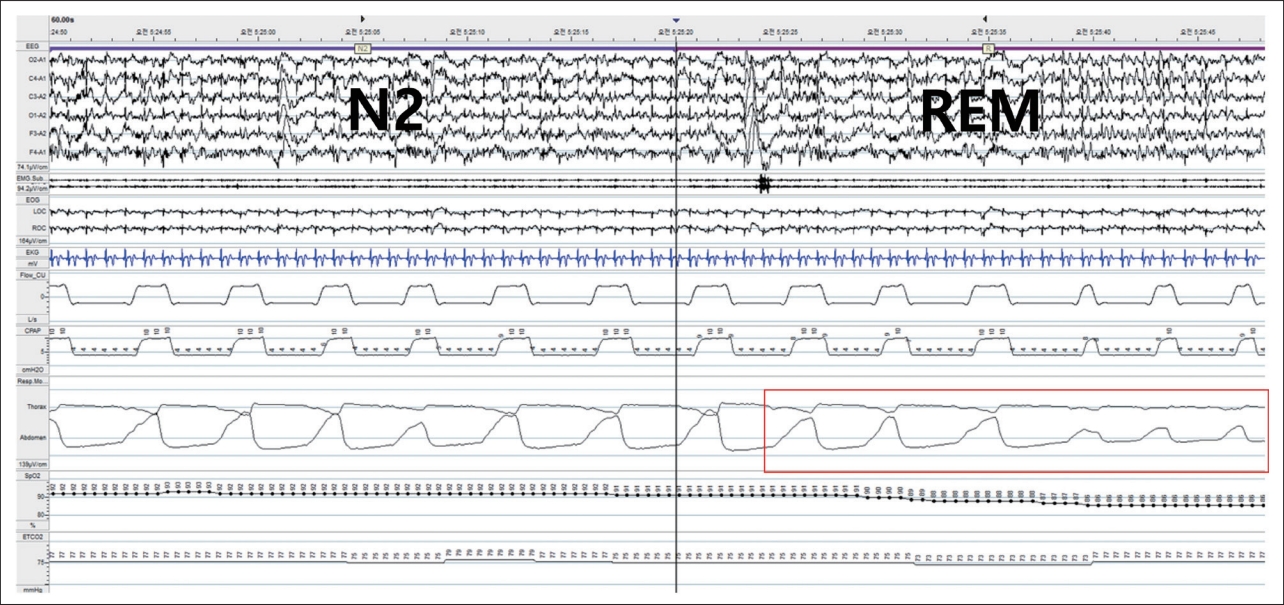
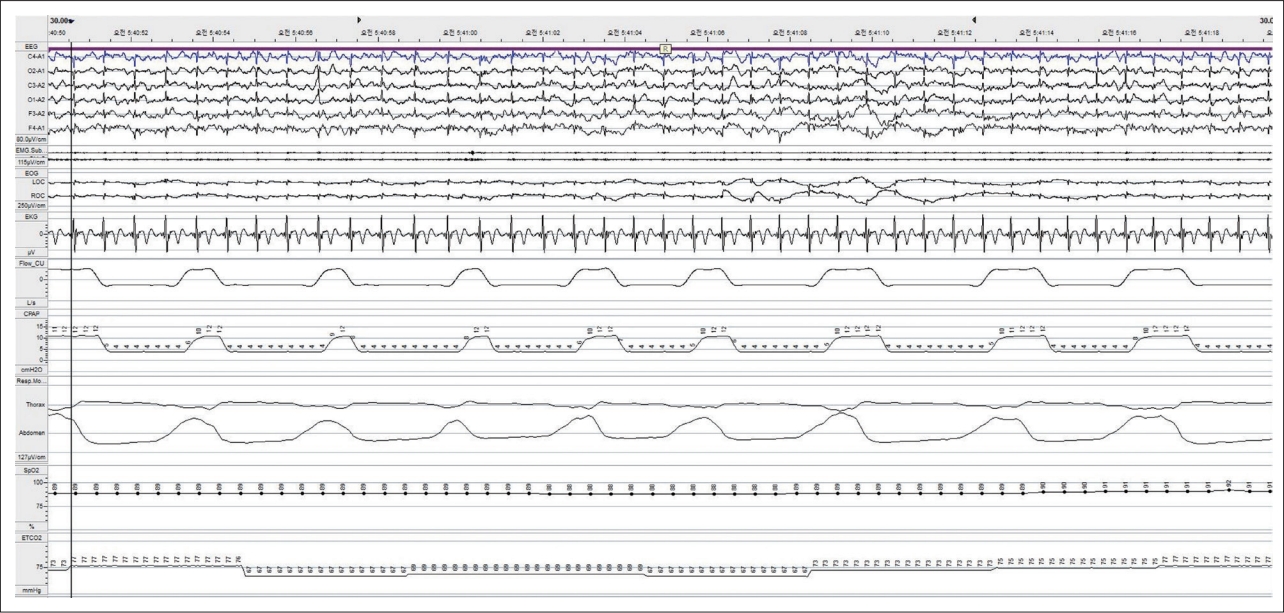
A 24-year-old male with kyphoscoliosis presented with aggravating dyspnea. He had surgically corrected with thoracic interbody fusion at age of 19. Initial daytime arterial blood gas test with oxygen 2 L/min showed: pH 7.31, PaCO2 88.5 mm Hg, PaO2 81.5 mm Hg, and HCO3- 36.8 mEq/L. The levels of PaCO2 during sleep were between 84 and 100 mm Hg. Investigations revealed hypoventilation syndrome with severe restrictive lung disease due to restrictive thoracic cage disorder (Fig. 1). Heart failure or pulmonary hypertension was excluded. Bilevel PAP (BPAP) was titrated focusing on improving ventilation based on daytime and morning arterial gas analysis. The patient was well tolerable to BPAP treatment and discharged with home oxygen therapy and nocturnal BPAP, inspiratory PAP (IPAP) 10 cmH2O, and expiratory PAP (EPAP) 5 cmH2O. Since BPAP was titrated insufficiently reflecting the sleep state, it was re-titrated with attended PSG although the patient did not complain of sleep-related symptoms. Under IPAP 10 cmH2O and EPAP 4 cmH2O, the patient was well ventilated during non-rapid eye movement sleep in supine position but during rapid eye movement (REM) sleep, respiration became unstable (Fig. 2). The final effective level of ventilatory support was reset to IPAP 12 cmH2O and EPAP 4 cmH2O accounting for the effects of REM sleep (Fig. 3). The patient snored lightly but had no sleep apnea.
Some patients with kyphoscoliosis have deformed chest walls with decreased chest wall compliance and weak diaphragm due to mechanically ineffective diaphragmatic movements, both leading to microatelectasis and alveolar hypoventilation [3]. Sleep itself causes decreased ventilatory response to hypoxia and increased PaCO2 which worsens hypoventilation and oxygen desaturation [4]. Since the diaphragm is the main inspiratory muscle during REM sleep, with the weakened diaphragm, when accessory muscle activities decrease during REM sleep, hypoventilation may be exacerbated secondary to insufficient respiratory efforts [5]. The decrease in ventilation during REM sleep further promotes microatelectasis and alveolar hypoventilation. A patient with kyphoscoliosis having low lung volume is more vulnerable to hypoxia, and alveolar hypoventilation may cause fatigue of the respiratory muscles and enter into a vicious cycle that promotes hypoventilation [3-5].
If possible, a patient with hypoventilation syndrome should be titrated with attended PSG because it is the only approach that adjusts the level of ventilatory support in real-time while assessing the effect of sleep state on respiration. Similar to this case, in many cases, since PSG cannot be performed immediately, further adjustment with attended PSG is warranted even after titration is done in a conventional way.
The requirement of informed consent was waived by the institutional review board (BPIRB 2022-04-038).