AbstractBackground and ObjectiveThe conventional criteria for body-mass index (BMI > 35 kg/m2) and neck circumference (NC > 40 cm) in the snoring, tiredness, observed apnea, high blood pressure, BMI, age, NC, and gender (STOP-Bang) Questionnaire may be too high to screen Korean obstructive sleep apnea (OSA) patients properly. We hypothesized that using a modified STOP-Bang Questionnaire with lower BMI and NC criteria may be more appropriate when screening South Korean patients with OSA. We aimed to evaluate the utility of the modified STOP-Bang Questionnaires and to compare it with that of conventional STOP or STOP-Bang Questionnaire.
Methods This was a cross-sectional single-center study done at Kyung Hee University Hospital at Gangdong. Consecutive patients who underwent polysomnography and had done the STOPBang Questionnaire between November 2010 and December 2017 were reviewed. We used alternative cut-off criteria for BMI as 30 kg/m2 and for NC as 36.3 cm.
Results A total of 778 patients was evaluated; 73.1% of them had some OSA [apnea-hypopnea index (AHI) > 5/hr] and 54.5% had moderate to severe OSA (AHI > 15/hr). The area under the curve (AUC) of the modified STOP-Bang was slightly larger than for the conventional STOP-Bang or STOP for having any OSA (AUC 0.787, 0.781, and 0.765, respectively) or for moderate to severe OSA (AUC 0.749, 0.747, and 0.721). The conventional STOP-Bang Questionnaire with a cut-off score of 3 identified all OSA and moderate to severe OSA patients with a sensitivity of 94.7% and 96.9%, respectively. The modified STOP-Bang showed improved sensitivity for any or moderate to severe OSA of 95.6% and 98.1%, respectively, with a decrease in exchange for lower specificity.
INTRODUCTIONThe STOP-Bang Questionnaire was first developed in 2008 and validated for screening patients for obstructive sleep apnea (OSA) surgery [1]. The questionnaire includes eight dichotomous items related to the clinical features of OSA: four subjective (STOP: snoring, tiredness, observed apnea, and high blood pressure) and four demographics items [Bang body-mass index (BMI), age, neck circumference (NC), and gender]. The cut-off criteria of 3 for STOP-Bang is known to indicate a high risk of OSA, with sensitivity and specificity of 83.6% and 56.4%, respectively [1]. Given its ease of use and high sensitivity, the STOP-Bang Questionnaire has been widely used in preoperative clinics, sleep clinics, the general population, and other special populations to detect patients at high risk of OSA [2].
A few studies evaluated the usefulness of the STOP-Bang Questionnaire for South Korean patients for screening OSA. One study showed that the STOP-Bang was the most useful tool among questionnaires, including the Berlin and Sleep Apnea of Sleep Disorder Questionnaire, with a sensitivity and specificity of 97.0% and 18.6% [3]. One recent study showed that the sensitivity and specificity of the STOP-Bang is 89.1% and 57.4%, respectively, with an area under the curve (AUC) of 0.809 [4].
Obesity is a well-known risk for OSA [5]. Because the questionnaire was initially developed and validated in western countries, the conventional STOP-Bang Questionnaire used BMI > 35 kg/m2 and NC > 40 cm as cut-off criteria to describe obesity [1]. Criteria for obesity in Asians are different from those for Caucasians; so using the identical criteria has been questioned when using the STOP-Bang in screening Asian patients for OSA [6-8]. Moreover, Asian OSA patients are generally known to be less obese even with a high apnea-hypopnea index (AHI) [9]. The conventional criteria for the BMI and NC in the STOP-Bang may be too high to screen Korean OSA patients properly.
We hypothesized that using modified STOP-Bang Questionnaire with lower BMI and NC criteria may be more appropriate when screening South Korean patients for OSA. In this study, we evaluated the utility of the modified STOP-Bang and compared it to the conventional STOP or STOP-Bang Questionnaire.
METHODSPatientsThis was a cross-sectional single-center study done at Kyung Hee University Hospital at Gangdong. We reviewed consecutive adult patients who underwent polysomnography (PSG) between November 2010 and December 2017. Those who failed to complete the questionnaire or underwent the split-night PSG were excluded. This study was approved by the Institutional Review Board of the Kyung Hee University Hospital at Gangdong (IRB No. 2019-07-011). Informed consent to participate was obtained from the enrolled patients.
ProceduresFor each patient, we reviewed demographics, results of sleep questionnaires, and PSG. Prior to the PSG, a patientŌĆÖs height, weight, and NC at the level of the cricoid cartilage was measured by the technician on duty.
An OSA diagnosis was made using standard PSG. The PSG was done using a digital polygraph system (Grass-Telefactor twin version 2.6, West Warwick, RI, USA) according to standard protocols. We recorded data from six electroencephalography channels (C3ŌĆōA2, C4ŌĆōA1, F3ŌĆōA2, F4ŌĆōA1, O3ŌĆōA2, and O2ŌĆōA1) according to the standard 10ŌĆō20 system in addition to two electrooculography channels and surface electromyography of chin and both anterior tibialis muscles. We scored the data manually according to the American Academy of Sleep Medicine Manual for the Scoring of Sleep and Associated Events [10]. Apnea was defined as a drop in peak thermal sensor excursion by at least 90% of the baseline value for at least 10 s. We defined hypopnea as a drop in the nasal pressure signal by at least 30% of the baseline value for at least 10 s, with at least a 4% reduction in oxygen saturation from the pre-event baseline. The AHI was defined as the number of apnea and hypopnea events per hour. We based the diagnosis of any OSA on an AHI of 5 or more events per hour. Moderate to severe OSA was classified based on the AHI values Ōēź 15/h.
Modified STOP-Bang Using Alternative BMI and NCWe used alternative BMI and NC criteria for the modified STOP-Bang. The alternative cut-off criteria for BMI and NC were set as follows: BMI as 30 kg/m2 based on World Health OrganizationŌĆÖs definition of severe obesity in Asia-Pacific population [11], and NC as 36.3 cm based on the definition suggested by the Korean Obesity Society [12].
StatisticsContinuous data are presented as the mean ┬▒ standard deviation. We used univariate and multivariate logistic regression analysis to evaluate the significance of each STOP-Bang and modified STOP-Bang Questionnaire components. We plotted receiver operating characteristics curves to assess the diagnostic accuracy of STOP, STOP-Bang, and modified STOP-Bang, using AHI cutoff points of 5 for any OSA and 15 for moderate to severe OSA. The greater AUC represents the better instruments. We calculated the sensitivity, specificity, positive predictive values, and negative predictive values of the STOP with a cut-off score of 2, and the STOP-Bang and modified STOP-Bang with a cut-off score of 3 or 4. The level of significance was set at p < 0.05. All statistical comparisons were done with SPSS (version 22.0, IBM Corp., Armonk, NY, USA).
RESULTSPatient characteristicsAmong the 880 consecutive adult patients who underwent PSG between November 2010 and December 2017, we analyzed a total of 778 patients who had completed the questionnaire and underwent PSG between November 2010 and December 2017. Overall, the mean age was 49.3 ┬▒ 13.3 years, and 75.7% were male. Mean BMI and NC were 26.7 ┬▒ 4.1 kg/m2 and 37.8 ┬▒ 3.9 cm, respectively. The proportion of those with any OSA was 73.1%, and 54.5% had moderate to severe OSA. Details of the sleep questionnaire and PSG findings are presented in Table 1.
Only 38 of the patients (4.9%) met the criteria of BMI > 35 kg/m2, and 139 (17.9%) met the criteria of BMI > 30 kg/m2. Prev alence of those who showed NC > 40 cm was 182 (23.4%), and 507 (65.2%) had NC > 36.6 cm (Table 2).
Significance of Each Component in Predicting Any or Moderate to Severe OSAThe most significant factor predicting any OSA was observed apnea [odds ratio (OR) 7.84, p < 0.001] followed by BMI > 35 kg/m2 (OR 7.04, p = 0.008), NC > 40 cm (OR 5.88, p < 0.001) and snoring (OR 5.43, p < 0.001), which was similar for predicting moderate to severe OSA. Tiredness and age > 50 years old showed no significant value in predicting overall OSA or moderate to severe OSA. Although alternative criteria for BMI and NC (BMI > 30 kg/m2 and NC > 36.6 cm) showed lower OR than did the conventional criteria, they still showed significant power in predicting OSA or moderate to severe OSA (Table 2).
Multivariate logistic regression analysis showed that the observed apnea has the most significant independent predictive value for any or moderate to severe OSA in both the conventional and the modified STOP-Bang. Tiredness, BMI, or NC did not have an independent predictive value in the conventional STOPBang. In the modified STOP-Bang, the BMI and NC using the alternative criteria showed independent significance; on the other hand, age and gender did not show independent significance (Supplementary Table 1 in the online-only Data Supplement).
Utility of the Modified STOP-Bang for Screening Any or Moderate to Severe OSAThe AUC of the modified STOP-Bang was slightly larger than that of the conventional STOP-Bang or STOP for any OSA (AUC 0.787, 0.781, and 0.765, respectively) or for moderate to severe OSA (AUC 0.749, 0.747, and 0.721) (Fig. 1, Table 3).
Using the conventional cut-off value of 3, the sensitivity of the modified STOP-Bang for overall OSA was higher than that of the conventional one for any OSA (95.6% vs. 94.72%, respectively) or for moderate to severe OSA (98.11% vs. 96.93%, respec-tively), but with lower specificity. When we increased the cut-off score to 4, the reduction in sensitivity was lower for the modified STOP-Bang and showed higher sensitivity than did the conventional STOP-Bang for any OSA (88.56% vs. 77.82%, respectively) or for moderate to severe OSA (91.96% vs. 82.27%, respectively), but with lower specificity. The STOP Questionnaire showed equivocal sensitivity and specificity than the STOP-Bang (Table 4).
DISCUSSIONWe evaluated the usefulness of the modified STOP-Bang using alternative BMI and NC criteria for screening OSA in South Korean patients. Unlike previous Korean studies that evaluated the validity of the conventional STOP-Bang [3,4], this study evaluated the utility of the modified STOP-Bang with alternative BMI and NC criteria. The conventional STOP-Bang Questionnaire with a cut-off score of 3 identified any OSA and moderate to severe OSA patients with a sensitivity of 94.7% and 96.9%, respectively. The modified STOP-Bang showed improved sensitivity for any or moderate to severe OSA to 95.6% and 98.1%, respectively, with a decrease in exchange for lower specificity.
Observed apnea had the highest predictive value among the STOP-Bang items, which was in line with the previous study [4]. Tiredness was not a significant factor, because we included biased patients who visited sleep clinics and underwent PSG. They all had sleep-related symptoms, and 89.5% of them complained of tiredness. In the general population, only 39.7% of the participants answered ŌĆ£yesŌĆØ to the tiredness component [8]. Symptoms related to OSA may be as important a predictor as are objective risk factors. The STOP Questionnaire, which mainly includes the symptom items, showed equivocal sensitivity and specificity compared to STOP-Bang.
The high cut-off criteria for BMI and NC has been an issue when using STOP-Bang in Asian populations. Mean BMI and NC in our patients were 26.7 ┬▒ 4.1 kg/m2 and 37.8 ┬▒ 3.9 cm, which were lower than those of the original Canadian cohort, with mean values of 30 kg/m2 and 39 cm. The proportion of patients exceeding BMI of 35 kg/m2 was only 6.3%, as in the previous study of South Koreans [12], which was lower than that of the Canadians (22.9%) [13]. A lower proportion of patients may increase the specificity of the questionnaire, but may decrease its sensitivity. Because Asians have OSA despite lower AHI [14], lower BMI criteria were evaluated in several Asian studies.
Two studies done in Singapore concluded that lowering the BMI criterion does not change the performance of the STOPBang Questionnaire. One study evaluated in-lab patients and found that lowering the BMI criterion to 30 kg/m2 increased the sensitivity in detecting moderate to severe OSA from 91.3% to 93.8% without a decrease in specificity [6]. The other study evaluated the general population and found that the alternative BMI criterion with 30 kg/m2 increased the sensitivity from 66.2% to 69.1%, with decreased specificity from 74.7% to 73.0% [8]. The degree of change of the sensitivity and specificity with the modified BMI criterion was similar to our results; however, the increased AUC suggests that the modified STOP-Bang in our study may be better in screening South Korean OSA patients. A recent study in China used a BMI cut-off value of 28 kg/m2, which increased the sensitivity of the modified STOP-Bang score Ōēź 4 in detecting moderate to severe OSA from 79.2% to 89.3% and reduced specificity from 43.6% to 38.2%. Although they found no significant difference in sensitivity, lowering the BMI cut-off showed the highest Youden index [15].
NC is known to be an independent predictor of OSA and its severity in snoring South Korean patients [16]. We applied a lower NC criterion following the Korean Obesity Society [12], and this increased the independent OR associated with any or moderate to severe OSA. However, 23.4% of the patients met the NC > 40 cm criterion, and 65.2% of the patients showed NC > 36.6 cm, which questions the validity of changing the NC criterion. A recent study showed that the optimal NC for predicting OSA in Singapore was 39 cm in males and 35 cm in females, which increased sensitivity from 71% to 83.4% and 32% to 84.6% respectively [17]. The NC criterion of 40 cm may be appropriate for screening OSA in South Korean males.
Although this study was a retrospective single-center study, it must be acknowledged that this work is the first to evaluate the feasibility of the alternative BMI and NC criteria in the STOPBang for Korean OSA patients. The true utility of the modified STOP-Bang should be validated in a general population.
The modified STOP-Bang using alternative criteria for BMI > 30 kg/m2 and NC > 36.6 cm increased AUC and sensitivity in predicting any OSA or moderate to severe OSA but decreased its specificity. Because of the high prevalence of undiagnosed OSA, the modified STOP-Bang should be applied to screen South Koreans with higher sensitivity.
Supplementary MaterialsThe online-only Data Supplement is available with this article at https://doi.org/10.17241/smr.2020.00591.
ACKNOWLEDGEMENTSThis work was supported by a grant from Kyung Hee University in 2019 (KHU-20192274).
REFERENCES1. Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, et al. STOP Questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 2008;108:812-21.
2. Chung F, Abdullah HR, Liao P. STOP-Bang Questionnaire: a practical approach to screen for obstructive sleep apnea. Chest 2016;149:631-8.
3. Kim B, Lee EM, Chung YS, Kim WS, Lee SA. The utility of three screening questionnaires for obstructive sleep apnea in a sleep clinic setting. Yonsei Med J 2015;56:684-90.
4. Kim KT, Cho YW. Real-world STOPBANG: how useful is STOPBANG for sleep clinics? Sleep Breath 2019;23:1219-26.
5. Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA 2000;284:3015-21.
6. Ong TH, Raudha S, Fook-Chong S, Lew N, Hsu AA. Simplifying STOPBANG: use of a simple questionnaire to screen for OSA in an Asian population. Sleep Breath 2010;14:371-6.
7. Pavarangkul T, Jungtrakul T, Chaobangprom P, Nitiwatthana L, Jongkumchok W, Morrakotkhiew W, et al. The Stop-Bang Questionnaire as a Screening Tool for obstructive sleep apnea-induced hypertension in Asian population. Neurol Int 2016;8:6104.
8. Tan A, Yin JD, Tan LW, van Dam RM, Cheung YY, Lee CH. Predicting obstructive sleep apnea using the STOP-Bang Questionnaire in the general population. Sleep Med 2016;27-28:66-71.
10. Berry RB, Brooks B, Gamaldo CE, Harding SM, Lloyd RM, Marcus CL, Vaughn BV. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, version 2.2. Darien, IL: American Academy of Sleep Medicine, 2015.
11. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157-63.
12. Kang JH, Ryu BY, Suh HS, Shim KW. Neck circumference as a simple obesity index. J Obes Metab Syndr 2002;11:142-9.
13. Chung F, Yang Y, Brown R, Liao P. Alternative scoring models of STOPBang Questionnaire improve specificity to detect undiagnosed obstructive sleep apnea. J Clin Sleep Med 2014;10:951-8.
14. Young T, Shahar E, Nieto FJ, Redline S, Newman AB, Gottlieb DJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the Sleep Heart Health Study. Arch Intern Med 2002;162:893-900.
15. Xia M, Liu S, Ji N, Xu J, Zhou Z, Tong J, et al. BMI 35 kg/m2 does not fit everyone: a modified STOP-Bang Questionnaire for sleep apnea screening in the Chinese population. Sleep Breath 2018;22:1075-82.
Fig.┬Ā1.Receiver operating curve for the three questionnaires compared to the reference line for (A) any OSA and (B) moderate to severe OSA. OSA: obstructive sleep apnea, STOP-Bang: snoring, tiredness, observed apnea, high blood pressure, body-mass index, age, neck circumference, and gender. 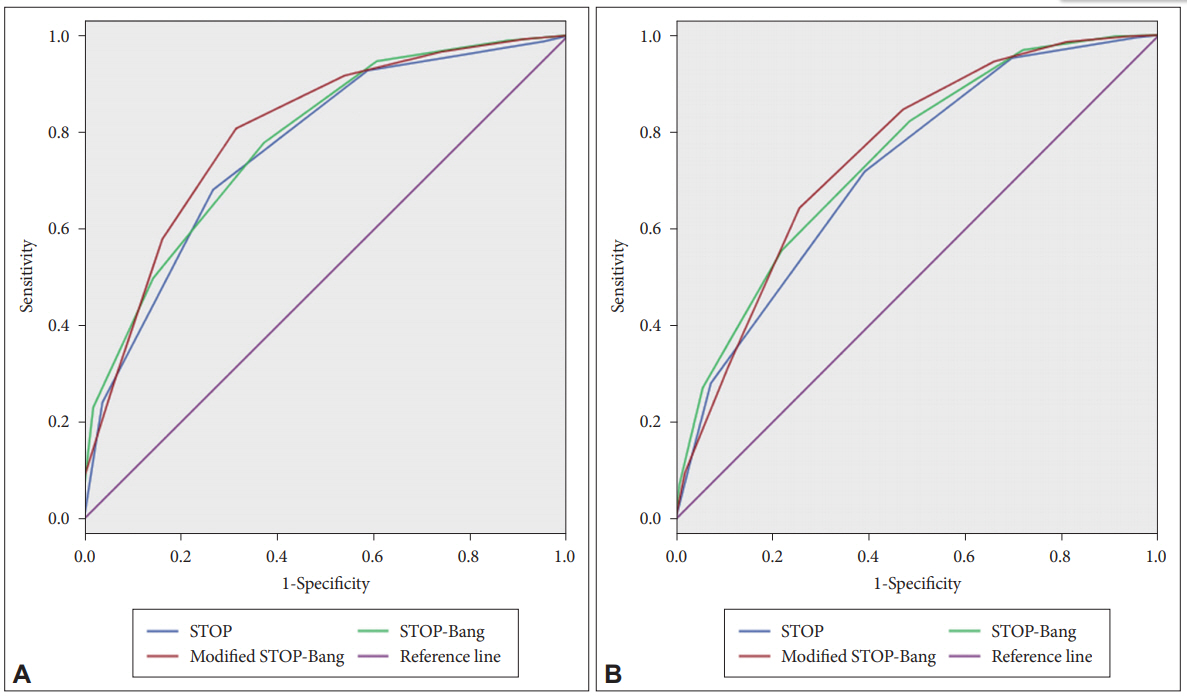
Table┬Ā1.Patient demographic, questionnaire score, and polysomnographic findings Table┬Ā2.Individual logistic regression for STOP-Bang variables predicting OSA Table┬Ā3.AUC for the STOP-Bang, modified STOP-Bang, and STOP
Table┬Ā4.STOP-Bang and modified STOP-Bang sensitivity, specificity for OSA |
|
||||||||||||||||||||||||||||||||||||||||||||||||||||