Psychological Distress During COVID-19: Its Association With Stress, Emotion Regulation, and Sleep
Article information
Abstract
Background and Objective
The COVID-19 pandemic has been linked to an increase in psychological distress and mental disorders worldwide. The objectives of this study were to investigate the correlates of psychological distress during the COVID-19 pandemic and explore whether the relationship between stress and psychological distress was mediated by cognitive emotion regulation strategies and sleep.
Methods
Four hundred ninety-six university students completed the Mental Health Inventory, the Insomnia Scale, the Cognitive Emotion Regulation Questionnaire, and the Perceived Stress Scale.
Results
Female gender and younger age were related to stress, sleep difficulties, and psychological distress. Stress was positively correlated with psychological distress and these two variables were associated with sleep difficulties, negative cognitive emotion regulation strategies (both positively), and positive cognitive emotion regulation strategies (inversely). In mediation analyses, there was a statistically significant positive direct/indirect impact of stress on psychological distress. The indirect pathways linking stress to psychological distress were: through an increase in negative cognitive emotion regulation strategies or a reduction in positive ones; through sleep difficulties; and through negative cognitive emotion regulation strategies and sleep. Female gender had a positive impact on sleep difficulty index, negative cognitive emotion regulation, and psychological distress.
Conclusions
The cognitive-emotional arousal associated with stress, as well as the maladaptive cognitive emotion regulation to cope with stress, may be implicated in the genesis and maintenance of sleep difficulties and distress during the pandemic. Strategies that include stress management, emotional self-regulation, and sleep hygiene should be implemented to promote the mental/psychological well-being of university students in future public health crises, such as the COVID-19 pandemic.
INTRODUCTION
The COVID-19 pandemic has affected more than 500 million people worldwide. The impact of the virus on health, the implementation of quarantine and physical isolation have contributed to fear of the disease, uncertainty about the future, significant suffering and psychological distress. An increased incidence of psychiatric disorders has been observed not only in vulnerable people, such as those with preexisting mental disorders and healthcare workers, but also among the general population, including in university students [1-3].
University students, in particular, were found to be more vulnerable to stress, anxiety disorders, and depression, especially among the younger population [2,3]. The mental health of Portuguese university students worsened during this period, as indicated by studies conducted by Pereira et al. [4] and Maia and Dias [5], which revealed higher levels of overall psychological distress, depression, anxiety, and stress among students during the pandemic compared to those assessed before it.
Regarding sleep quality, studies also indicate that a large majority of the general population during the COVID-19 pandemic reported at least one sleep difficulty, with frequent awakenings being one of the most described [6]. Additionally, there is evidence suggesting that sleep patterns changed, and sleep quality worsened among university students during the COVID-19 [7].
Stress is one of the main risk factors of mental disorders, and research shows that the pandemic context is a significant factor that is likely to increase its levels. It is therefore important to study the impact of the pandemic on stress-inducting paradigms [8] and emotion regulation strategies and insomnia/sleep difficulties are relevant and sensitive factors to consider due to their possible impact on stress experience and mental health [9-14].
The relationship between stress, sleep difficulties, and psychological distress are well-established in the literature. Stress is a precipitant factor for sleep difficulties/insomnia [15-17]; stress and sleep difficulties/insomnia are associated with and both constitute risk factors for mental disorders, including depression and anxiety [1-4,6,18]. Taking these findings into account, it is possible that sleep difficulties mediate the association between stress and psychological distress. In fact, a study conducted during the COVID-19 pandemic by Liu et al. [18] observed that insomnia mediated the relationship between perceived stress and depression, meaning that insomnia strengthens the relationship between stress and depressive symptoms.
Emotion regulation plays an important role in human adjustment to adverse life events [19-21]. Cognitive emotion regulation consists of a set of cognitive strategies for dealing with the excessive emotional arousal that arises when faced with threatening or stressful life events [20]. Thus, there is empirical evidence that both non-adaptive (e.g., rumination, self-blame, catastrophizing, thought suppression) and adaptive cognitive emotion regulation strategies (e.g., positive refocusing, positive reappraisal) are related respectively to negative emotions/psychological distress and positive emotions [19-23]. Additionally, emotional regulation also plays a crucial role in dealing with cognitive-emotional arousal triggered by adverse life events, which is a relevant maintenance factor for sleep difficulties and insomnia [17].
Some studies conducted before the COVID-19 pandemic have explored the relationships between stress and sleep difficulties in university students, focusing on emotional psychological distress and/or emotion regulation strategies as mediators. A study performed in 2018 by Amaral et al. [23] analyzed the relationship between stress and sleep difficulties, along with the mediating roles of negative perseverative thinking, rumination, and negative affect. The study found a direct effect of perceived stress on sleep difficulties and an indirect effect of perceived stress on sleep difficulties through rumination, negative affect, and the effect of rumination on negative affect. Another study by Amaral et al. [24] conducted in 2015 with a sample of university students revealed that rumination partially mediated the relationship between perceived stress and overall sleep difficulties.
In a study carried out on a sample of the Norwegian general population during the COVID-19 pandemic, Haver et al. [25] observed a moderation effect of suppression (positively) and positive reappraisal (negatively) on the relationship between stress and psychological distress.
The present study aims to 1) examine whether stress, cognitive emotion regulation strategies, and sleep difficulties are associated with psychological distress during the COVID-19 pandemic and 2) explore whether the relationship between stress and psychological distress is mediated by cognitive emotion regulation strategies and sleep.
One of our hypotheses is that psychological distress during the COVID-19 pandemic may be related to the levels of experienced stress, sleep difficulties, the high use of non-adaptive cognitive emotion regulation strategies to deal with adversity, and the low use of positive strategies. Additionally, we hypothesize that the severity of stress is expected be related to an increase in psychological distress, and this link may be strengthened by maladaptive cognitive emotion regulation strategies (adaptive ones may have a protective effect) and sleep difficulties as mediating variables of this association.
METHODS
Procedures and Sample
This cross-sectional study is part of a research project approved by the Ethics Committee of the Faculty of Medicine at the University of Coimbra (reference: CE-156/2020). Participants provided informed consent and subsequently completed an online questionnaire during a period of mandatory COVID-19 pandemic confinement (between January 28, 2021 and May 24, 2021), which was disseminated through the competent bodies of universities and on social networks.
The study included 496 university students from various institutions in Mainland Portugal and the Islands (Azores and Madeira), aged between 18 and 27 years (mean = 22.99; SD = 2.27). Of these, 106 (21.4%) were male and 390 (78.6%) were female; 97.8% were single, 94% were of Portuguese or dual nationality, 99.2% were attending undergraduate or integrated master’s programs, and the remaining 0.8% were enrolled in doctoral or postgraduate programs.
Instruments
The psychological distress dimension of the Portuguese version of the Mental Health Inventory (MHI) [26] that comprises the items of anxiety, depression, and loss of control subscales was used. Its items are measured on a 5-point Likert scale ranging from 1 (never/almost never) to 5 (always/almost always) and a higher the score on this inventory indicates better mental health status (lower levels of psychological distress).
To evaluate sleep difficulties, we utilized 3 items of the Insomnia Scale [27,28] related to difficulties in initiating sleep (DIS; Did you have difficulties in falling asleep?), difficulties in maintaining sleep (DMS; Did you wake up several times during the night or experience problems getting back to sleep?), and early morning awakenings (EMA; Did you wake up too early in the morning and couldn’t get back to sleep?), which were answered on a 5-point scale, from 1 (never/almost never) to 5 (almost always/always). Additionally, a sleep difficulty index (SDI) was computed by summing the scores of these 3 items, where higher scores indicate more sleep difficulties.
The Portuguese version of the Cognitive Emotion Regulation Questionnaire (CERQ-36) [20,29] was used to assess eight cognitive emotion regulation strategies: namely, positive reappraisal and planning, positive refocusing, putting into perspective, acceptance, rumination, blaming others, self-blame, and catastrophizing [20-29]. Each item is rated on a scale from 1 (almost never) to 5 (almost always) and higher scores reflect a greater use of the respective cognitive emotion regulation strategy. The sum of the scores from the first four subscales corresponds to the positive or adaptive cognitive emotion regulation dimension (CERP), while the sum of the scores from the last four subscales corresponds to the negative or maladaptive cognitive emotion regulation (CERN) [2,20,27-30].
To assess perceived stress over the past month, including aspects such as unpredictability, uncontrollability, and overload associated with daily life situations, the Perceived Stress Scale (PSS) [30,31] was applied. It consists of 10 items with response options ranging on a scale of 0 (never) to 4 (always) [31]. A higher score indicates higher levels of perceived stress. The PSS has been widely used in studies during the pandemic. In the sample of the present study, the PSS showed concurrent validity with the Pandemic Stress Index [32], which assesses COVID-19 pandemic stress (behavioural change: r = 0.235; overall pandemic impact on daily life: r = 0.328; psychosocial distress: r = 0.515, total: r = 0.517, p < 0.01 for all).
Statistical Analysis
To analyze the data, we utilized IBM SPSS Statistics (Version 27; IBM Corp., Armonk, NY, USA).
Students who answered Insomnia Scale questions with the response options “frequently” (3 times or more per week) and “almost always/always,” which were rated as 4 and 5, respectively, were considered to have DIS, DMS, and EMA with some severity. The cut-off points of one standard deviation above/below the mean were also appropriately applied to determine the percentage of students with global sleep difficulties (SDI), stress (PSS), and psychological distress (MHI) with some severity. We employed Pearson’s and Spearman’s correlation coefficients, as appropriate, to investigate the relationship between the variables and Cohen’s criteria [33] to analyze their magnitude: low (r = 0.10 to 0.29), moderate (r = 0.30 to 0.49), and high (r = 0.50 to 1.0).
Student’s t-test and Mann–Whitney U-test were used appropriately. To assess the effect size magnitude (Student’s t-test), Cohen’s d was used: 0.2 = small, 0.5 = medium, and 0.8 = large [33,34]. To investigate the link between perceived stress (variable X) and psychological distress (variable Y), using CERN or CERP (M1) and SDI (M2) as mediators, a multiple serial mediation analysis was conducted (Hayes’ Model 6) [35], using the PROCESS macro for SPSS (version 3.5.3, 2017–2022). The choice of variables to be included in the mediation models considered statistically significant associations observed in the previous analyses. Gender was therefore chosen as a covariate controlled in the analysis. Bootstrap confidence intervals (95% CIs) for indirect effects were calculated repeatedly using 5000 samples, estimating the model in each sample, calculating indirect effects, and deriving final confidence intervals. An indirect effect is nonzero with a 95% CI if the value zero is not contained within it. If zero is contained within the 95% CI, then the indirect effect is not statistically different from zero.
RESULTS
Descriptive Statistics
Students with high levels of sleep difficulties (with an SDI score one standard deviation or more above the mean) were 19.2% (n = 95), and those who reported DIS, DMS, and EMA (answered 3 times or more per week or almost always/always) were 41.1% (n = 204), 24.8% (n = 123), and 15.9% (n = 79), respectively. Students with high levels of stress (with a PSS score one standard deviation above the mean) were 16.7% (n = 83), and those with high levels (scores equal to or lower than one standard deviation below the mean, as lower MHI scores indicate a worse state of mental health) of loss of control were 16.7% (n = 83), of anxiety were 16.9% (n = 84), of depression were 16.1% (n = 80), and of psychological distress were 18.3% (n = 91).
Relationship of Variables with Gender and Age
Women, compared to men, had significantly higher levels of symptoms for stress, sleep difficulties (SDI, DIS, and DMS), depressive symptoms, anxiety, loss of control, and psychological distress; on the other hand, men exhibited higher levels of blaming others. The magnitude of gender differences in the means of these variables ranged from slight to moderate (from d = 0.118 to d = 0.620) (Table 1).
Younger age was significantly associated with higher levels of stress, DIS, and overall psychological distress, depression, anxiety, and loss of control. It was also associated with lower use of positive cognitive emotion regulation strategies, particularly positive reappraisal and planning, and putting things into perspective (Table 2).
Interrelationships between Variables
The intercorrelations between the variables are described in Table 2.
Regarding psychological distress and its dimensions, they were significantly and robustly associated with stress and moderately/highly with higher levels of overall sleep difficulties (SDI), DIS, DMS, and EMA.
Low to moderate positive relationships between stress and sleep difficulties (SDI, DIS, DMS, and EMA) were also observed.
Concerning cognitive emotion regulation, psychological distress and its dimensions, stress, and sleep difficulties (SDI, DIS, and DMS) consistently correlated with higher use of negative cognitive emotion regulation strategies (CERN; rumination, self-blame, and catastrophizing) and lower use of positive cognitive emotion regulation strategies (CERP; positive reappraisal and planning; positive refocusing). Psychological distress, its dimensions, and stress were also slightly associated with lower use of putting things into perspective/lower use of perspective-taking. Additionally, psychological distress and depressive symptoms were related to blaming others.
Concerning EMA, they showed a slight positive association with the mentioned negative cognitive emotion regulation strategies and a lower use of positive reappraisal and planning. DMS also showed a positive and modest relationship with blaming others.
Relationship between Stress and Psychological Distress; The Mediating Roles of CERN and SDI
The multiple serial mediation analysis was applied to explore the link between Perceived Stress Scale total score (PSS-T) and psychological distress, using CERN (M1) and SDI (M2) as mediators, and gender as a covariate (Table 3 and Fig. 1). The variables in the model explained approximately 78.5% of the variance in psychological distress (R2 = 0.7850; F(4,491) = 448.2334, p < 0.001), with high stress, CERN, SDI, and gender (female) significantly contributing to its explanation. A statistically significant direct impact (c’) of stress on the increase in psychological distress was observed. The total effect of X on Y (c) as well as the total indirect effect (c-c’) were also statistically significant. Three indirect pathways linking stress to psychological distress were found. In one of these paths, the perceived stress led to an increase in CERN, which in turn resulted in an increase in psychological distress levels (X-M1-Y). On the other, stress triggered an increase in SDI levels, which resulted in an increase in psychological distress (X-M2-Y). Finally, stress led to an increase in CERN, which in turn determined an increase in SDI, which had an impact on the increase of psychological distress (X-M1-M2-Y). The covariate gender (female) had a significant effect on decreasing CERN and increasing SDI and psychological distress.

Mediation model of the effect of global stress on psychological distress, with CERN and SDI variables as mediators, and gender as a covariate
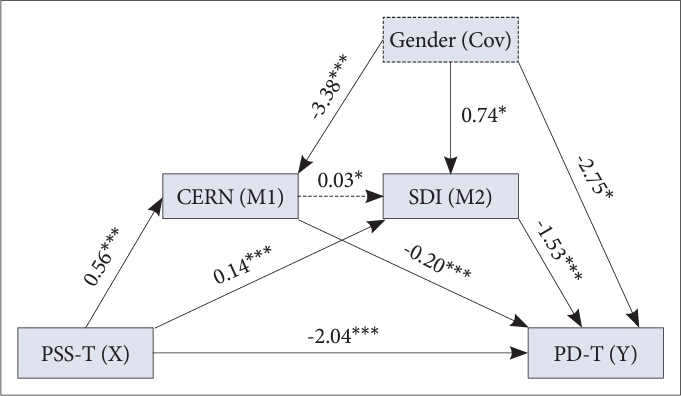
Diagram of the multi-factor serial mediation analysis between PSS-T (X) and PD-T (Y) using CERN and SDI as mediators and gender as a covariate. Arrows drawn with a continuous line: statistically significant links; Values on the arrows: regression coefficient. *p < 0.05; ***p < 0.001. M1, mediator 1; M2, mediator 2; Cov, covariate.
Relationship between Stress and Psychological Distress; The Mediating Roles of CERP and SDI
The multiple serial mediation model (Model 6) [23] was also applied to analyze the link between PSS-T and psychological distress, using CERP (M1) and SDI (M2) as mediators, with gender as a covariate (Table 4 and Fig. 2). These variables in the model explained approximately 78.4% of the variance in psychological distress (R2 = 0.7843; F(4,491) = 446.4041, p < 0.001), with high stress, CERP (inversely), and SDI significantly contributing to its explanation. A statistically significant direct link was observed between perceived stress and an increase in psychological distress (c’). The total effect of X on Y (c) as well as the total indirect effect (c-c’) were also statistically significant. Two indirect paths linking stress to psychological distress were found. In one path, perceived stress led to a decrease in CERP, a variable that had an impact on reducing levels of psychological distress, thus acting as a protective factor for mental health (X-M1-Y). On the other path, stress led to an increase in SDI levels, which, in turn, resulted in an increase in psychological distress (X-M2-Y). The covariate gender (female) had an effect on increasing SDI and psychological distress.

Mediation model of the effect of global stress on psychological distress with CERP and SDI variables as mediators, and gender as a covariate

Diagram of the multi-factor serial mediation analysis between PSS-T (X) and PD-T (Y) using CERP and SDI as mediators and gender as a covariate. Arrows drawn with a continuous line: statistically significant links; Arrows with a discontinuous line: nonstatistically significant links; Values on the arrows: regression coefficient. *p < 0.05; ***p < 0.001. M1, mediator 1; M2, mediator 2; Cov, covariate.
DISCUSSION
One of the objectives of this study was to examine whether sleep, stress, and cognitive emotion regulation strategies were associated with psychological distress during the COVID-19 pandemic and the results support these relationships. Another aim was to analyze the processes that link stress to psychological distress and the results of the study also show that cognitive emotion regulation strategies and sleep difficulties play an important role in the association between stress and psychological distress.
In the present sample of presumed healthy university students, approximately 18% of the participants revealed psychological distress of some severity, among whom: 16% had symptoms of depression, 17% had symptoms of anxiety, and 17% experienced loss of control. Students with high levels of stress accounted for 16.7% of the sample. Those who experienced severe sleep difficulties constituted 19.2%, while those reporting severe DIS, DMS, and EMA were 41.1%, 24.8%, and 15.9%, respectively.
A pre-pandemic longitudinal study [36], which assessed the levels of sleep difficulties in Portuguese university students at three different time points, using items similar to those in the present study to evaluate DIS and DMS, revealed the presence of DIS in 8%–9.7% of students; and DMS in 13.4%–17.2% of respondents. Another study [23] on sleep difficulties in Portuguese university students conducted before the pandemic, using items with a similar formulation to the present study but with dichotomous response options (no/yes), reported rates of 29.8% for DIS, 27.9% for DMS, and 30.9% for EMA. In the present study, we observed consistently higher levels of sleep difficulties than in the first study and of DIS than in both studies [23,36], which leads us to hypothesize that there may have been an increase in sleep difficulties among university students during the pandemic period and that this could have a negative impact on psychological distress. The increase in stress and psychological distress during the COVID-19 pandemic is also a highly consistent finding in the literature [1-3,6,7], and described in Portuguese university students [4,5].
It is important to understand the factors that may be associated with the psychological distress increment during the COVID-19 pandemic. The findings of the present study indicated that psychological distress (overall, depression, anxiety, and loss of control) during the pandemic was related to stress, sleep difficulties (overall, DIS, DMS, and EMA), high use of negative cognitive emotion regulation strategies (particularly rumination, self-blame, and catastrophizing), and low use of positive cognitive emotion regulation strategies (especially positive reappraisal and planning, positive refocusing, and putting into perspective). Our previous work, performed with the sample of the present study, also revealed that these variables distinguished the high psychological distress group from the low and moderate psychological distress groups [37]. These results confirm the findings reported by Amaral et al. [23] in a study conducted in 2018, which showed that stress, global sleep difficulties, high use of negative cognitive emotion regulation strategies (particularly rumination, self-blame, and catastrophizing), together with lower use of positive cognitive emotion regulation strategies (particularly positive reappraisal and planning, positive refocusing, and putting into perspective) are associated with increased negative affect in university students.
Women and younger students are at a higher risk of developing stress, sleep difficulties, and psychological distress. Regarding cognitive emotion regulation, younger students, compared to older students, use fewer positive cognitive emotion regulation strategies, particularly putting things into perspective, and positive reappraisal and planning. Men, compared to women, use blaming others more. Amaral and Collegues [23,38] also observed that male university students made greater use of the blaming others strategy to regulate their emotions, while female students reported more sleep difficulties (DMS and EMA) and higher levels of perceived stress [23,38]. The association between female gender and psychological distress (symptoms of anxiety and depression) is a highly consistent finding in the literature, including studies carried out among university student populations in various countries [2,39,40]. With regard to age, younger students may be more affected by the transition to university, which has been shown to generate considerable stress and increase psychological distress in students [39], which have been exacerbated by the social and learning challenges caused by COVID-19 pandemic [2].
Focusing on the processes linking stress to psychological distress, through the mediation of cognitive emotion regulation strategies and sleep difficulties (while controlling for the gender effect), it was observed that there was a direct relationship between stress and sleep difficulties, along with four statistically significant indirect pathways. Thus, it was evident that a reduction in the use of positive cognitive emotion regulation strategies, as well as an increase in the use of negative strategies, mediates the relationship between stress and psychological distress. In another way, sleep was the mediator, meaning that stress results in a decrease in sleep quality, which in turn contributes to higher levels of psychological distress. Finally, stress amplifies psychological distress when mediated by the impact of negative cognitive emotion regulation strategies on sleep difficulties, meaning that stress is related to greater use of negative cognitive emotion regulation strategies, which in turn exacerbate sleep difficulties, leading to an increase in psychological distress.
To our knowledge, no previous study has examined the role of cognitive emotion regulation strategies and sleep in the relationship between stress and psychological distress during the COVID-19 pandemic, which is a strength of our study. However, the results are consistent with the findings of the survey with Norwegians which showed that suppression and cognitive reappraisal moderated the association between COVID-19 stress and psychological distress [25]. The results also confirm the findings of two studies carried out on Portuguese university students during the pre-pandemic period, regarding the role of sleep difficulties in the association between stress and psychological distress. The results indicate that there is a direct effect of stress on sleep difficulties [25], that negative cognitive emotion regulation strategies (rumination) partially mediate the association between stress and sleep difficulties [30], and that negative cognitive emotion regulation strategies and negative affect mediate the association between stress and sleep difficulties [25]. They also confirm the conclusions of Liu et al. [18] with Chinese medical students during the pandemic, which indicated that insomnia mediated the relationship between perceived stress and depression.
A limitation of the present study is its cross-sectional design, which did not allow for the exploration of true causal relationships between the variables. Future studies should employ a longitudinal design, and it is worth emphasizing that research conducted in the context of future health crises should consider the importance of conducting pre-crisis and post-crisis pandemic assessments or during-pandemic various time points assessments.
In conclusion, the results of the present study suggest that stress is associated with psychological distress, has an impact on its increasing, and that the high use of maladaptive cognitive emotion regulation strategies and the low use of adaptive ones, as well as poor sleep quality strengthen the association between them. So, the results draw attention to the importance of stress as a precipitant of sleep difficulties and psychological distress during the COVID-19 pandemic, as well as the determining role of sleep difficulties in psychological distress. Deficient emotion regulation strategies in coping with cognitive-emotional arousal associated with stress may be implicated in the maintenance of sleep difficulties and psychological distress. The lower use of positive cognitive emotion regulation strategies may amplify the levels of stress, psychological distress, and sleep difficulties, and can be particularly detrimental when associated with the higher use of negative cognitive emotion regulation strategies. This relationship between positive and negative cognitive emotion regulation strategies may be relevant to the maintenance of stress, sleep difficulties, and psychological distress.
These findings are consistent with those of other studies conducted prior to the pandemic, highlighting the relevance of these variables and processes in determining psychological distress at any periods of life, even in the most adverse phases, such as the COVID-19 pandemic. It is interesting to note that the variables in our study (gender, SDI, stress, and CERP/CERN) explained a great percentage of the variance in psychological distress (over 78%). However, a bidirectional relationship is also plausible, as psychological distress, and psychiatric disorders are among the primary causes of insomnia [34], and both can lead to higher levels of stress.
The results of the present study may have clinical implications. Interventions aimed at promoting mental/psychological wellbeing in Portuguese university students during public health crises like the COVID-19 pandemic should be considered. Special attention should be given to the fact that younger students and women are vulnerable groups for the development of high levels of stress and psychological distress. To reduce students’ susceptibility to developing psychological distress, interventions should focus on reducing stress, promoting healthy sleep habits, reducing the use of negative emotion regulation strategies, and promoting positive ones.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Author Contributions
Conceptualization: João Carlos Pinto de Sousa, Maria João de Castro Soares. Formal analysis: João Carlos Pinto de Sousa, Maria João de Castro Soares. Investigation: João Carlos Pinto de Sousa, Maria João de Castro Soares. Methodology: João Carlos Pinto de Sousa, Maria João de Castro Soares. Project administration: António Ferreira de Macedo e Santos, Maria João de Castro Soares. Supervision: António Ferreira de Macedo e Santos, Maria João de Castro Soares. Writing—original draft: João Carlos Pinto de Sousa. Writing—review & editing: António Ferreira de Macedo e Santos, Maria João de Castro Soares, Ana Paula Monteiro Amaral, Ana Telma Fernandes Pereira.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Funding Statement
None
Acknowledgements
The authors are very grateful to all Universities that collaborate in the study and to all the students who participate in it.


