Sleep Effort and Insomnia Severity: The Role of Bedtime Procrastination
Article information
Abstract
Background and Objective
We aimed to investigate the mediating role of bedtime procrastination in the relationship between sleep effort and insomnia severity in this study.
Methods
We included 497 university students in this study. All the participants completed the sociodemographic data form, Glasgow Sleep Effort Scale (GSES), Insomnia Severity Index (ISI), Depression-Anxiety-Stress Scale-21 (DASS-21), and Bedtime Procrastination Scale (BPS). We divided the participants into groups, according to their GSES and BPS scores, those with high-low sleep effort and those with BP (+) and BP (-), respectively. We compared the variables in these groups. Finally, we analyzed the mediating role of bedtime procrastination in the relationship between sleep effort and insomnia severity.
Results
The mean age of the participants was 20.41 ± 1.83 years. ISI, BPS, and DASS-21 were statistically significant in the group with high sleep effort (p < 0.01). Among the psychometric instrument scores, the highest correlation with GSES was with ISI, and then there was a statistically significant positive correlation with DASS-21. In addition, there was a statistically significant positive correlation between GSES and BPS. Bedtime procrastination played a partial mediation role in the relationship between sleep effort and insomnia severity.
Conclusions
Bedtime procrastination partially mediated the relationship between sleep effort and insomnia severity. Therapists should consider sleep effort and bedtime procrastination on their agenda in cognitive behavioral therapy sessions for insomnia.
INTRODUCTION
Sleep is crucial for memory, emotion regulation, and physical health [1]. However, studies have found that insomnia is common among university students [2]. A recent study found clinical insomnia and poor sleep quality in 15.9% and 74% of university students in Turkey, respectively [3]. University students experience many negative consequences of insomnia, such as fatigue, poor learning and memory, and difficulties maintaining attention and regulating emotions [4-6]. Consequently, their academic performance and social life are affected [7,8]. Therefore, it is crucial to understand the factors that contribute to insomnia or poor sleep quality among university students.
Physiological, psychological, and environmental variables such as gender, body weight, chronotype, and psychological stress affect sleep quality in young people [9-12]. Recent studies revealed a significant relationship between sleep hygiene behaviors and sleep quality. For example, bedtime habits and preferences have been shown to determine sleep quality; using electronic media before bedtime, doing more activities after 9 p.m., turning off the lights late, and going to bed late have frequently been associated with poor sleep quality [13-17].
Sleeping is a process that should be spontaneous, like the beating of the heart or breathing [18]. Sleep effort is sleep-related performance anxiety. It includes various components such as cognitive (e.g., I must sleep) and behavioral (e.g., trying too hard to sleep). Good sleepers make no effort to sleep, while poor sleepers usually make a lot of effort to sleep [3]. Those who make a great effort to sleep overthink about sleep, do not practice good sleep hygiene and may use over-the-counter sleep medications. In addition, they are likely to postpone their bedtime because they believe they cannot sleep. As a result, excessive sleep effort leads to the development and maintenance of insomnia [19].
Bedtime procrastination is defined as not going to bed at the desired time even though no external conditions prevent it [20]. Routines, such as brushing teeth, setting the alarm, or immersive activities before sleeping such as accessing social media or e-mail, playing an online game, and online chatting, can cause bedtime delay [21,22]. Bedtime procrastination may impair sleep quality and is a risk factor for insomnia in college students. People who are evening-type and with lower self-control are likely to exhibit more bedtime procrastination behaviors [23]. Bedtime procrastination may also be defined as an avoiding behavior from unwanted distress, which exacerbates mental illnesses. Bedtime procrastination may function similarly to safety behaviors in patients with insomnia [24]. For example, individuals who make a great effort to sleep (high sleep-related performance anxiety) may avoid going to bed and delay bedtime even more by predicting that they will not be able to sleep when they go to bed [25]. Such avoidance behaviors contribute to the development and maintenance of insomnia.
In light of the above information, in this study, we examined the mediating role of bedtime procrastination in the relationship between sleep effort and insomnia severity. To the best of our knowledge, this is the first study on this topic. Our hypotheses were as follows: 1) Bedtime procrastination behavior and insomnia are more severe in individuals who make great effort to sleep. 2) Individuals who make great effort to sleep or those with bedtime procrastination have higher levels of depression, anxiety, and stress. 3) There is a positive correlation between sleep effort, bedtime procrastination, depression, anxiety, and stress levels. 4) Bedtime procrastination mediates the relationship between sleep effort and insomnia severity.
METHODS
Participants and Procudure
This study included students of the Gaziantep University, Turkey, Faculty of Health Sciences and Faculty of Arts and Sciences. We used the G*Power 3.1.9.7 for Windows XP (https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower) to calculate the sample size. The confidence interval was α = 0.05, the test power (1-β) was 0.95, the effect size was dz:0.1886792, and the minimum sample size should have been 367 participants according to power analyze.
We conducted this study between 25 December 2022 and 10 January 2023. We included 497 university students in the study. All the participants signed informed consent and then completed the sociodemographic data form, Glasgow Sleep Effort Scale (GSES), Insomnia Severity Index (ISI), Depression-AnxietyStress Scale-21 (DASS-21), and Bedtime Procrastination Scale (BPS). We obtained ethical approval from the Clinical Research Ethics Committee of Gaziantep University (Date: 21.12.2022, decision no:2022/467). All the procedures were conducted in accordance with ethical rules and the principles of the Declaration of Helsinki.
Data Collection Tools
Sociodemographic data form
We designed a sociodemographic data form with questions on the participants’ information such as age, gender, marital status. In addition, there were questions about their weekday and weekend sleep patterns.
Glasgow Sleep Effort Scale (GSES)
Bromfield and Espie created GSES to measure sleep effort. The scale has seven items and a 3-point Likert structure [19]. Turkish version of GSES was adapted and showed a reliable and valid scale in the Turkish university population [3]. We used Turkish GSES to assess sleep effort in this study because it is the only Turkish instrument about sleep effort. The total score ranges from 0 to 14, and higher scores indicate higher sleep effort [3]. We found a high internal consistency coefficient (Cronbach’s α = 0.782). High sleep effort can be categorized as a cut-off value of 6 points and above [3]. In this study, we divided the participants into two groups according to this value, those with high and low sleep effort.
Insomnia Severity Index (ISI)
ISI consists of 7 items and evaluates insomnia severity in the last two weeks [26]. It is the literature’s most widely used scale to evaluate insomnia severity [26,27]. We used ISI to assess insomnia severity in this study. The total score ranges from 0 to 28. A high score indicates severe insomnia, and ISI showed good internal consistency (Cronbach’s α = 0.816) in this study.
Bedtime Procrastination Scale (BPS)
BPS has nine items and a 5 Likert (1 = almost never, 5 = almost always) structure. Items 2, 3, 7, and 9 are reverse-scored, and the total score ranges from 0 to 45. Higher scores are related to more bedtime procrastination [20]. BPS was adapted into Turkish by Yılmaz Dinç et al. [28]. We chose the BPS to measure bedtime procrastination since it is the only scale in Turkish. We divided the participants into two groups those who delay bedtime (BP (+), BPS > 27) and those who do not delay bedtime (BP (-), BPS ≤ 27). We made this distinction according to this study’s median value 27 of BPS. The Cronbach’s coefficient in this study was 0.61. Sample items were “If it is time to turn off the lights at night, I do it immediately” and “I do not go to bed on time.” [20].
Depression-Anxiety-Stress Scale-21 (DASS-21)
DASS-21 has seven items each to measure depression, anxiety, and stress dimensions [29]. Each item is scored between 0 and 3. A total score of between 0 and 21 is obtained, and higher scores reflect more depression, anxiety, and higher stress levels. It is the most widely used tool in the literature recently to determine the level of depression, anxiety, and stress. Therefore, we used DASS-21 to asses the depression, anxiety, and stress levels of the participants. In this study, we calculated a robust Cronbach’s α (0.936) for DASS-21.
Statistical Analysis
Results were analyzed using SPSS 23.0 (IBM Corp., Armonk, NY, USA). We presented descriptive statistics as mean, standard deviation, and percentage. We examined whether the data were normally distributed with the skewness and kurtosis values. We used the Student’s t-test for intergroup comparisons. We used Spearman and Pearson correlation methods for correlation analysis. We divided participants into two groups with and without bedtime delay according to the median value of BPS (> 27) and according to their GSES, high and low sleep efforts, and compared the variables. Pearson’s correlation was used to determine the relationship between the relevant variables. A p-value < 0.05 was considered statistically significant.
We used PROCESS macros in SPSS 23.0 (IBM Corp., Armonk, NY, USA) for mediation analyses [30]. Analyses were tested for indirect effects using 5000 bootstrapped samples [31,32]. The hypothesized model examined whether bedtime procrastination mediated the relationship between sleep effort (GSES scores) and insomnia severity (ISI score). We considered pathways as statistically significant if the 95% CI did not include zero.
RESULTS
Characteristics of All the Participants
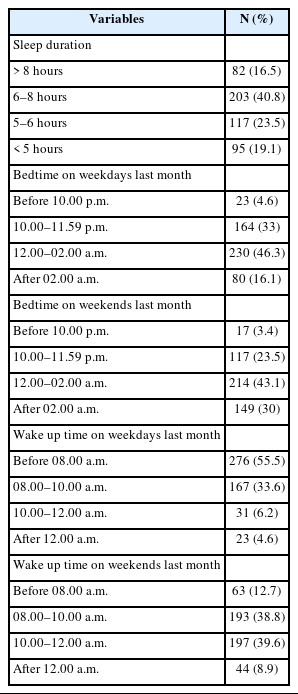
Tables 1 and 2 show the participants’ sociodemographic variables, scale means, and sleep routines. The mean age of the participants was 20.41 ± 1.83. The age range of the participants was 17–33 years. Most participants were female and single, and more than half lived with their families. The mean ± standard deviation values of BPS and GSES were 27.12 ± 4.62 and 7.38 ± 4.38, respectively. Approximately 1 out of 5 participants had a sleep duration of fewer than 5 hours, and bedtime was after 02.00 a.m. on a weekday. On the other hand, one of the three participants was after 02.00 a.m. on the weekends. The waking up times on weekdays and weekends, as well as the bedtime hours, were also different. While nearly half of the participants got up before 08:00 a.m. on weekdays, 12% of all the participants got up before 08:00 a.m. on weekends.
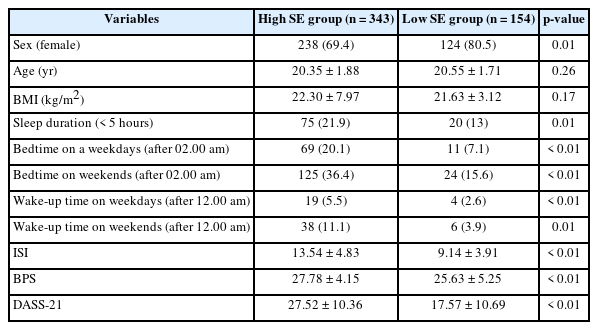
Comparison between High and Low Sleep Effort Group
Table 3 displays a comparison between the high and low-sleep effort groups. As a result, 69% of all participants (343/497) were in the high sleep effort. The number of female participants was statistically significantly higher in the group with low sleep effort than in the group with high sleep effort. There was no statistically significant difference between the two groups in age and Body Mass Index (BMI) (p = 0.26, p = 0.17). The number of participants with have less than 5 hours of sleep duration was higher in the high sleep effort group. ISI, BPS, and DASS-21 scores were statistically significantly higher in the group with high sleep effort (p < 0.01).
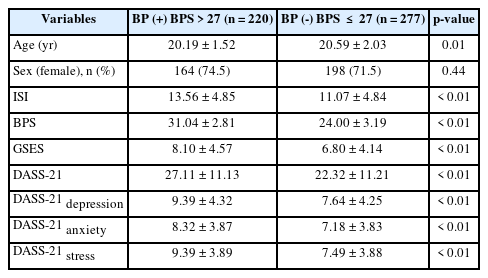
Comparison between Bedtime Procrastination (+) and Bedtime Procrastination (-) Groups
Table 4 shows a comparison between BP (+) and BP (-) groups. As a result, 44.3% of all participants were in the BP (+) group. There was no statistically significant difference between the two groups in sex (p = 0.44). On the other hand, there was a statistically significant age difference; the mean age was lower in BP (+) group than in the BP group (-). In the group BP (+), ISI, BPS, GSES, and DASS-21 scores were statistically significantly higher (p < 0.01).
Correlations between Psychometric Instruments
We found correlations between psychometric instruments. There was a significant positive correlation between all scales. The highest correlation with GSES had a positive correlation with ISI (r = 0.570), and then there was a statistically significant positive correlation with DASS-21 (r = 0.545). In addition, there was a statistically significant positive correlation between GSES and BPS (r = 0.269).
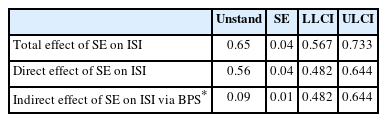
The Mediating Role of Bedtime Procrastination on Sleep Effort and Insomnia Severity
We found a significant association between sleep effort and insomnia severity (c path or total effect = 0.65, sleep effort [SE] = 0.04, p < 0.001). Further, we observed a positive association between sleep effort and bedtime procrastination (a-path, excessive sleep effort was associated with more bedtime procrastination behavior) and between bedtime procrastination and insomnia severity (b-path, with more bedtime procrastination behavior associated with more insomnia severity). The indirect effect (ab) of bedtime procrastination behavior on insomnia severity was also significant (Table 5); the direct effect, including the mediator, was reduced but still significant (c’ = 0.56, SE = 0.04, p < 0.001). Therefore, bedtime procrastination partially mediated the relationship between sleep effort and insomnia severity.
DISCUSSION
To the best of our knowledge, this is the first study to evaluate the association between bedtime procrastination and sleep effort among university students. In this study, first, we aimed to test the hypothesis that individuals with high sleep effort have more severe insomnia and higher levels of depression, anxiety, and stress and that they exhibit bedtime procrastination behavior. Second, we investigated whether bedtime procrastination may mediate the relationship between sleep effort and insomnia severity. The main findings of this study were that bedtime procrastination and insomnia severity were higher in the group with high sleep effort. Individuals with high sleep effort had shorter sleep duration and went to bed later. The behavior of bedtime procrastinating was higher in younger individuals, and those who bedtime procrastinated had higher sleep effort, insomnia severity, depression, anxiety, and stress scores. Finally, bedtime procrastination partially mediated the relationship between sleep effort and insomnia severity.
The most critical point in the onset of insomnia is stress [33]. Moreover, maladaptive behaviors and cognitive distortion related to insomnia lead to chronic insomnia. Sleep effort is an essential issue among maladaptive behavior and cognitive errors related to sleep [19]. Most insomniacs make a great effort to sleep, making insomnia catastrophic. This situation exacerbates insomnia and can shorten sleep duration. Our results showed that the sleep duration was shorter and the severity of insomnia was higher in those with high sleep effort. In addition, individuals with high sleep effort had some strategies to sleep better. For example, they may delay their sleep time even more by going to bed and waiting for hours to sleep or by deliberately not going to bed to get more sleep [24].
The other main findings in this study were that individuals with high sleep effort slept later on weekdays and weekends, and they delayed their bedtime more. The relationship between sleep effort and procrastination has never been investigated before. A previous study determined that delaying bedtime mediated the relationship between anxiety and sleep problems [24]. Individuals with high anxiety exhibit avoidance behaviors or some safety-providing behaviors to avoid unwanted emotions or thoughts [34]. Sleep effort means sleep-related performance anxiety. Individuals with high sleep effort may also engage in some safety-providing or avoidance behaviors. For example, individuals with high sleep effort may refrain from going to bed to avoid confirming their fear of falling asleep quickly. Individuals with high sleep effort may delay their bedtime more simply because they cannot sleep. However, some activities they do during this time can make their minds more alert and make it harder for them to fall asleep. On the other hand, they may have postponed their bedtime more, thinking that getting more sleep is needed to have a good sleep. In both cases, delaying bedtime increases the burden of insomnia for individuals with high sleep effort.
Many studies have found that insomnia predicts depression, anxiety, and stress [35]. It is also known that insomnia is the most common sleep disturbance in depression and anxiety disorders [36]. High sleep effort, one of the most important mechanisms underlying insomnia, can also increase depression, anxiety, and stress levels. In this study, depression, anxiety, and stress levels were higher in those with high sleep effort. Therefore, some participants may have experienced insomnia due to depression or anxiety disorders. Many depressed and anxious patients may have delayed their bedtime because they could not sleep or escape unwanted emotions. It may have been a confounding factor in this study. Studies found that bedtime procrastination was associated with problematic internet use, low self-control, and predicted insomnia in university students [37,38]. In addition, bedtime procrastination shortens sleep duration, leads to insufficient sleep, and triggers depression and anxiety [39]. In this study, we found that the severity of insomnia and depression, anxiety, and stress scores were higher in the group of participants who postponed bedtime in parallel.
Limitations and Future Recommendations
This study has some limitations. First, we only included university students and there was no data collection for older/younger people, so the results cannot be generalized. Second, most of the participants were females. Third, the sample size was small. Fourth, we used self-psychometric scales; they lack objective evaluation, and the results cannot fully demonstrate causality. Despite all this, for the first time, this study reported the relationship between sleep effort and bedtime procrastination. In the future, studies with larger samples and structured clinical interviews examining the relationship between sleep effort and bedtime procrastination are needed.
Conclusion
Bedtime procrastination partially mediated the relationship between sleep effort and insomnia severity. Based on the results of this study, clinicians should screen individuals with insomnia for sleep effort and bedtime procrastination with GSES and BPS, respectively. For individuals with high sleep effort, the reasons for the delayed bedtime should be evaluated, and they should be informed about sleep hygiene rules, including bedtime procrastination. Therapists should put sleep effort and bedtime procrastination on their agenda in cognitive behavioral therapy sessions for insomnia.
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Authors’ Contribution
Conceptualization: Omer Faruk Uygur. Data curation: Aynur Bahar. Formal analysis: Omer Faruk Uygur. Methodology: Omer Faruk Uygur, Aynur Bahar. Statistical analysis: Omer Faruk Uygur. Writing—original draft: Omer Faruk Uygur, Aynur Bahar. Writing—review & editing: Omer Faruk Uygur.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Funding Statement
None.