INTRODUCTION
Sleep is an altered consciousness phenomenon that occurs not only in humans but also across all animal species and is essential in maintaining good health and quality of life [1]. The quality of sleep has a profound effect on mental health, especially on emotional regulation [2]. It is well known that sleep plays a major role in the processing of daily emotions, consequently, poor sleep quality triggers negative emotions and causes emotional dysregulation [3]. Therefore, poor sleep quality is a potential risk factor for the development of mental disorders [2].
A negative stimulus elicits a wide range of corrective responses; however, when the responses fail or are inadequate, negative emotion occurs [4]. Positive psychology believes that self-control can trigger positive emotions [5], and if an individual fails to trigger positive emotions through self-control activities, emotional control difficulties arise. These emotional regulation difficulties are closely related to depression [6]. Examples of human emotional regulation behaviors in positive psychology include eating a hearty meal and exercising [7] while unhealthy emotional regulation behaviors include smoking and drinking alcohol [8].
Sleep problems are core symptoms of depression. Approximately 75% of depressed patients have insomnia or hypersomnia symptoms, and the sleep problems cause huge distress with a major impact on the quality of life [2]. However, although there is a high correlation between sleep quality and depression, poor sleep quality does not necessarily cause depressive symptoms [9]. For instance, insomnia does not necessarily mean a major depressive disorder, and many people with poor sleep quality do not develop mood disorders [3,10,11]. We, therefore, assume that several variables mediate the process from poor sleep quality to depression. Among the possible parameters are an individual’s biological vulnerability, and an individual’s choices of emotion control activities.
Therefore, this study aimed to evaluate the connection between individual emotional self-regulation activities, sleep quality, and depressive symptoms. Using mediation analysis, we analyzed community survey data to investigate if there is a correlation between daily emotion regulation activities (such as eating breakfast, exercise, smoking, and drinking), sleep quality, and depression. We further examined whether daily emotional regulation activities have a mediating effect on the development of depression due to poor sleep quality using a structural equation model.
METHODS
Study Population and Data Collection
For this study, we used data from the 2018 Korea Community Health Survey (KCHS), conducted by the Korea Centers for Disease Control and Prevention. The KCHS is a nationwide, cross-sectional survey with a study population from a multi-stage cluster sampling, stratified by primary sample units of civilian, non-institutionalized Korean households by geographic area, age, and gender groups. The survey is conducted annually, and it collects information through face-to-face and a paper-assisted personal interview between interviewers and respondents. The sample size for the KCHS is 900 subjects in each of 253 community units, including 16 metropolitan cities and provinces. Because the population sample is selected using a probability proportional to the sampling methods and, weighted by statisticians who performed post-stratification and considered the non-response rates, samples are representative of the Korean population.
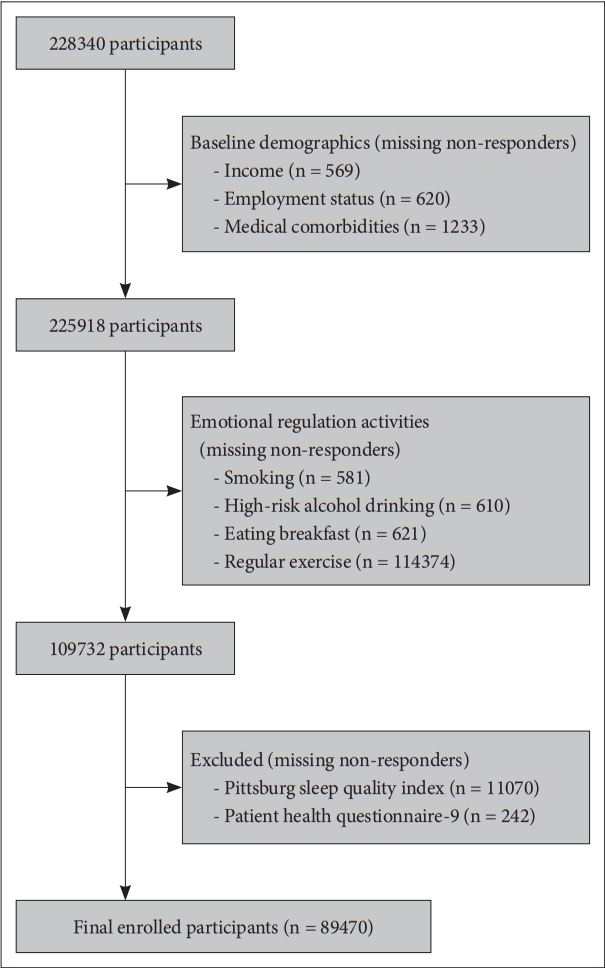
This study included individuals aged 19 years or older. Of the 228340 total survey participants, respondents who did not provide data on their income, employment status, smoking status, alcohol consumption, meal activities, exercise behavior, and scale for sleep quality, or scale for depressive symptoms were excluded. Finally, a total of 89470 eligible participants were included in this study (Fig. 1).
Sleep Quality and Depressive Symtoms
Sleep quality was measured using the Korean version of the Pittsburg Sleep Quality Index (PSQI-K) which included several sleep-related behaviors; in 2018, PSQI-K was included in the KCHS for the first time. The PSQI is a 19-items self-reported questionnaire that measures the quality and patterns of sleep over a 1-month duration [12]. This study consisted of 7 sleep components: C1, subjective sleep quality; C2, sleep latency; C3, total sleep duration; C4, sleep efficiency; C5, sleep disturbance; C6, use of sleep medication; and C7, daytime dysfunction. The PSQI-K has been validated and shown to have adequate reliability [13]. Total PSQI score has been widely used before to measure sleep quality. In this paper, the lower the sleep quality, the higher the total PSQI score, and the higher the sleep quality, the lower the total PSQI score, the higher total PSQI score was regarded as poor sleep quality.
Depressive symptoms were measured using the Patient Health Questionnaire-9 (PHQ-9) that has been widely used in population-based studies because it’s self-reporting and simple. The Korean version of PHQ-9 has also been validated and shown high reliability [14].
Emotional Regulation Activities
The emotional regulation activities measured in this study were as follows: regular breakfast, regular exercises, smoking, and alcohol drinking. The number of days that people had eaten breakfast in the previous week among people who reported eating their meals regularly was used to define regular breakfast. Among the participants who answered to exercise behavior, the most recent one-month regular exercise was defined as regular exercise. We defined alcohol drinking-related behavior with a subscale of The Korean version of Alcohol Use Disorders Identification Test to measure how much alcohol was consumed in the most recent month. The variable of smoking was classified as snoking every day, occasionally smoking, and not smoking.
Statistical Analysis
Since the data from KCHS were collected using stratified, clustered, and systematic sampling, complex survey dataset analysis methods were used while following the guidelines of KCHS analysis, which were published by the Korea Centers for Disease Control and Prevention [15]. Descriptive statistics were used to identify the participants’ baseline characteristics. Logistic regression analysis was done, and the receiver operating characteristic (ROC) curve was drawn to evaluate the feasibility of sleep quality in predicting depressive symptoms. To explore the effects of emotion regulation activities that mediate the link between sleep quality and depressive symptoms, correlation analyses were done. We used statistical methods in a way that created structural equation methods and validated this model. Since there are many missing values, the maximum likelihood with the missing value method is used for estimation. We used a different stepping algorithm in nonconcave regions for maximization. Optimization was done by 300 maximum iterations. Covariance structure used the following: sex, age, household income level, employment status, and current medical comorbidity which could affect sleep quality (diabetes mellitus, hypertension, cerebrovascular disease, asthma, allergic rhinitis, atopic dermatitis). Differences were considered statistically significant at ap-value less than 0.05. Statistical analyses were performed using STATA version 16 (STATA Corp., College Station, TX, USA).
This study was approved by the Institutional Review Board of St. Vincent’s Hospital in Korea (VC21ZASI0245).
RESULTS
Baseline Participants' Characteristics
The demographics and baseline characteristics of participants are presented in Table 1. The mean age of the participants was 54.52 ± 17.58 years, and 44.78% of the participants were male. The average monthly household income of the participants was 46.88 ± 35.84 million won, and 61.58% of participants were currently employed. 32.68% of the participants had medical comorbidities. 16.01% said they smoke every day, 1.32% said they smoke occasionally and 82.66% said they don’t smoke. 32.55% of the patients said they didn’t drink alcohol, 16.73% said they drink less than once a month, 8.91% said they drink twice or four times a month, 19.86% said they drink two to three times a week, and 8.14% said they drink more than four times a week. Among those who said they eat regularly, 11.33% said they had never eaten breakfast in the past week, 11.33% said they had eaten once, 3.51% said they had eaten twice, 4.44% said they had eaten twice, 2.50%, 5.65%, and 1.46% said they had eaten six times. Of the participants who responded to exercise behavior, 39.20% reported exercising regularly.
Correlation between Sleep Quality and Depressive Symptoms
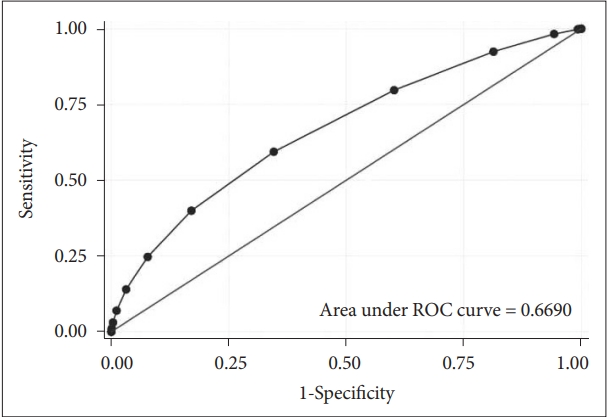
When the logistic regression analysis was performed to see how well the total score of PSQI predicted the degree of depressive symptoms measured by PHQ-9, the odds ratio was 1.40 (95% confidential interval [CI] 1.40–1.41, p < 0.001). Based on these results the ROC curve was drawn, and the area under the ROC curve was measured at 0.6690, which is shown in Fig. 2.
Correlations between Different Types of Emotional Regulation Activities, Sleep Quality, and Depressive Symptoms
Prior to drawing the Structural Equation Model, Pearson correlation analysis was performed to evaluate the association between each variable, and the results are shown in Table 2. Emotion regulation activities were significantly correlated with PSQI total scores but were not significantly correlated with PHQ-9 total scores.
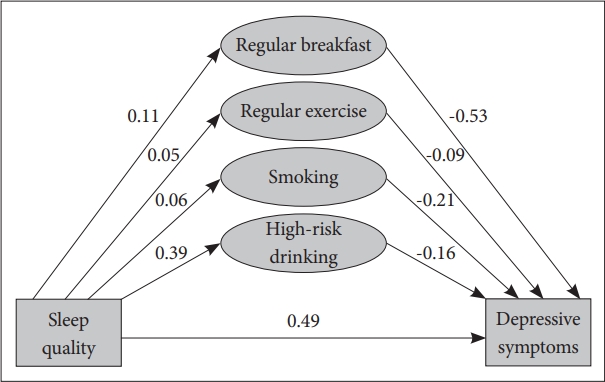
The structural equation model was drawn to evaluate how emotional regulation activities mediated between sleep quality and depressive symptoms, and the results are shown in Fig. 3 and Table 3. The direct effects of the total PSQI scores on each emotional control behavior are as follows: the correlation between the total score of PSQI and eating breakfast was 0.11 (95% CI, 0.10–0.11), the effect for regular exercise was 0.05 (95% CI, 0.05–0.05), the effect for smoking was 0.06 (95% CI, 0.06–0.06). Between PSQI and PHQ-9, the mediating effect of eating breakfast was -0.53 (95% CI, -0.56–-0.51) and the mediating effect of regular exercise was -0.09 (95% CI, -0.12–-0.05). The mediating effects between PSQI and PHQ-9 of smoking and alcohol drinking were -0.21 (95% CI, -0.26–-0.17) and -0.16 (95% CI, -0.17–-0.15), respectively. All the results were significant with a p-value < 0.0001.
DISCUSSION
This study aimed to identify the role of everyday emotional regulation activities in the development of depressive symptoms as a result of poor sleep quality. Based on our results, we found emotional regulation activities to be a potent mediator between sleep quality and depression.
Further, there was a significant correlation between PSQI total score and PHQ-9 total score, but it was shown that ROC under the area was 0.66 and poor sleep quality predicted only about 66% of the depressive symptoms. This is consistent with the existing report that although sleep disturbance is one of the core symptoms of depression, poor sleep quality does not necessarily mean major depression.
The positive correlation between the total PSQI score and emotion regulation activities indicated a correlation between poor sleep quality and regular breakfast eating habits, that is, people try to eat breakfast more regularly to regain regularity in life after experiencing poor sleep quality. In the same context, the tendency to exercise more regularly correlated the poorer sleep quality, although the correlation coefficient was not statistically significant.
The study found that poor sleep quality increases the frequency of alcohol use, and this is consistent with the existing study results [16,17]. However, emotion regulation activities alone do not seem to directly correlate with depressive symptoms. Previous studies on the relationship between alcohol/nicotine use and depression showed that there was no correlation, similarly, in this study, there was no correlation between the degree of depression and frequency of alcohol and nicotine use.
On the other hand, the application of the structural equation model of the relationship showed that emotion regulation activities had a protective effect on the process of going from poor sleep quality to depression. Eating breakfast was found to prevent depression to a very high degree, and regular exercise had the least protective effect on depression, unexpectedly. Meanwhile, smoking and alcohol drinking have also been shown to have antagonistic effects on depressive symptoms, this is consistent with previous studies and our clinical experience of increased smoking and drinking levels when experiencing negative mood associated with depressive symptoms [18,19].
This study demonstrates that routine emotion regulation activities are protective of the sleep disturbance to depression process. Eating breakfast regularly seems to have a preventive effect on the process that leads to major depression in patients with poor sleep quality. Based on the results of this study, there was a positive correlation between poor sleep quality, and regular breakfast eating habits, which could prevent depression despite poor sleep quality; several other studies have also concluded that skipping breakfast has a high correlation with depression, and regular breakfast prevents depression [20-26]. This can be termed as part of human self-regulatory adaptive behavior for preventing depression.
Interestingly, our study results confirm our assumption that people with poor sleep quality will increase alcohol consumption or drink alcohol to relieve their negative emotion study. A similar trend is also observed in smoking, and several studies have shown that smoking and drinking can be a kind of emotional control behavior for overcoming depressed moods [27-31]. However, addictive substances such as alcohol and nicotine harm health, making it difficult to recommend them as a means of relieving negative emotions. Therefore, based on the findings, real-world clinicians can advise patients that eating breakfast and exercising regularly could prevent depression.
Although this paper does not publish its results, it has shown that these emotion regulation activities have little effect in preventing suicidal ideation. Therefore, our daily emotion regulation activities measured in this paper are not absolute depressive symptoms prevention approaches and psychiatric intervention is essential for patients with suicidal ideation who visit the primary clinic.
There are many limitations to this study. First, there may be a reporting bias because it was a survey study based on self-reporting. Furthermore, biological effects such as family history and bipolarity that can affect depression must be considered; this could not be considered in this study. There is also a large amount of missing data even though the interviews were conducted by trained interviewers. Since the survey was conducted by laymen who did not have clinical experience in sleep medicine, rather than experienced interviewers who specialized in measuring PSQIs, there may be errors such as confusion in the morning/afternoon. Therefore, although the data were double-checked and the time was corrected, the data accuracy may be low. In addition, education levels were excluded from the covariate, which was thought to be a factor predicting education levels due to the low level of education and the high young population in Korea for decades. In addition, since the study is not aimed at accurate diagnosis and medical records of actual patients, there are many clinical application limitations. Therefore, verifying the findings through actual clinical trials will be necessary.
Nevertheless, to the best of our knowledge, this is the first study to investigate how daily emotion regulation activities correlate with sleep quality and depressive systems. Since this study is a large-scale epidemiological study based on community samples, the findings of this study can be considered as a relatively good reflection of the population.
In conclusion, daily emotional regulation activities, especially eating breakfast regularly, have a protective effect on the process of developing depressive symptoms in patients with poor quality. We plan to conduct further studies on how such emotion regulation activities can prevent depressive symptoms.